When you’ve been coughing up thick, foul-smelling mucus every day for months-or years-it’s easy to think it’s just a stubborn cold or smoking-related irritation. But if you’re producing at least 30 milliliters of yellow or green sputum daily, along with constant fatigue and shortness of breath, you might be dealing with bronchiectasis. It’s not just a cough. It’s a chronic lung condition where your airways have permanently widened and lost their ability to clear mucus. And without the right management, it gets worse over time.
What Bronchiectasis Actually Does to Your Lungs
Your lungs are designed to trap dirt, germs, and mucus in tiny hairs called cilia, then sweep them out. In bronchiectasis, those airways are damaged-stretched, scarred, and floppy. They can’t move mucus properly. So it pools. And when mucus sits still, bacteria grow. That triggers infection, which causes more inflammation, which damages the airways even more. It’s a cycle: mucus builds up → infection flares → airways get worse → more mucus builds up. This isn’t something that shows up overnight. Most people don’t realize they have it until they’ve been sick for years. The damage often starts after a bad pneumonia, whooping cough, or even a childhood infection. By the time symptoms become obvious, the structure of the airways has already changed. That’s why a chest CT scan is the gold standard for diagnosis: it shows airways that are at least 1.5 times wider than the blood vessels next to them.The Three Big Symptoms You Can’t Ignore
There are three signs that point strongly to bronchiectasis:- A daily productive cough that produces more than 30mL of sputum-often thick, sticky, and smelly.
- Repeated lung infections, sometimes with fever or chills.
- Shortness of breath that gets worse over time, even with light activity.
Why Airway Clearance Isn’t Optional-It’s the Foundation
Doctors will tell you this over and over: if you skip airway clearance, nothing else works as well. Antibiotics won’t prevent reinfection if mucus is still sitting in your lungs. And even the best meds won’t stop lung function from declining. The goal? Get that mucus out. Daily. No exceptions. There are several proven techniques:- Active Cycle of Breathing Techniques (ACBT): A sequence of breathing control, deep breathing, and huff coughing. It’s free, requires no equipment, and can be done anywhere.
- Positive Expiratory Pressure (PEP) devices: Like the Aerobika® or Flutter valve. You breathe out against resistance, which helps loosen mucus. These cost $150-$200 and are covered by some insurance.
- High-frequency chest wall oscillation vests: These vibrate your chest while you breathe. They’re expensive ($5,000-$7,000) and usually reserved for people who can’t do other techniques.
How to Huff Correctly (It’s Not Just Coughing)
Most people think coughing hard is enough. It’s not. Huff coughing is different. It’s a controlled, forceful exhale-like you’re trying to fog up a mirror. There are three types:- Medium huff: Breathe in normally, then huff out as if you’re steaming glasses.
- Low huff: Breathe in deeply, then huff out with your mouth open, like you’re blowing out a candle far away.
- High huff: Take a big breath, then huff hard and fast from deep in your chest.
Antibiotics: When and How to Use Them
Antibiotics aren’t for every cough. But in bronchiectasis, they’re a key part of long-term control. There are two main approaches:- Prophylactic (preventive): Taking a low dose of azithromycin (250-500mg) three times a week. This reduces flare-ups by 32% compared to placebo, according to the EMBRACE trial. It also has anti-inflammatory effects, not just antibacterial.
- On-demand: Taking antibiotics only during an exacerbation-when sputum turns darker, increases in volume, or you feel worse. This is common, but risky.
What About Nebulizers and Other Treatments?
Nebulized hypertonic saline (7% salt water) is a simple, powerful tool. It draws water into the mucus, making it thinner and easier to cough out. Most people use 3mL once or twice daily. It’s cheap, safe, and works for most. Dornase alfa (Pulmozyme), a drug used in cystic fibrosis, can also help break down DNA in thick mucus. It’s not FDA-approved for bronchiectasis, but many doctors prescribe it off-label-and studies show it improves clearance. Bronchodilators (like albuterol) don’t help much on their own. But when used before airway clearance, they can open the airways slightly and make clearing mucus 28% more effective.Real People, Real Struggles
On patient forums, the most common complaint isn’t the cough-it’s the time. “Doing 20 minutes of airway clearance twice a day while working two jobs and raising kids? Impossible,” wrote one user on the NHS forum. Another said they missed two weeks of therapy after a family emergency-and within a month, they were back in the hospital. But the success stories are powerful too. One man went from nine hospitalizations a year to just one after starting daily hypertonic saline and ACBT. Another switched from a $6,000 oscillating vest to a $180 PEP device-and saw the same results. The biggest hurdle? Consistency. People who stick with it for six months report a 4.2/5 satisfaction rating for symptom control. But only 2.9/5 for convenience.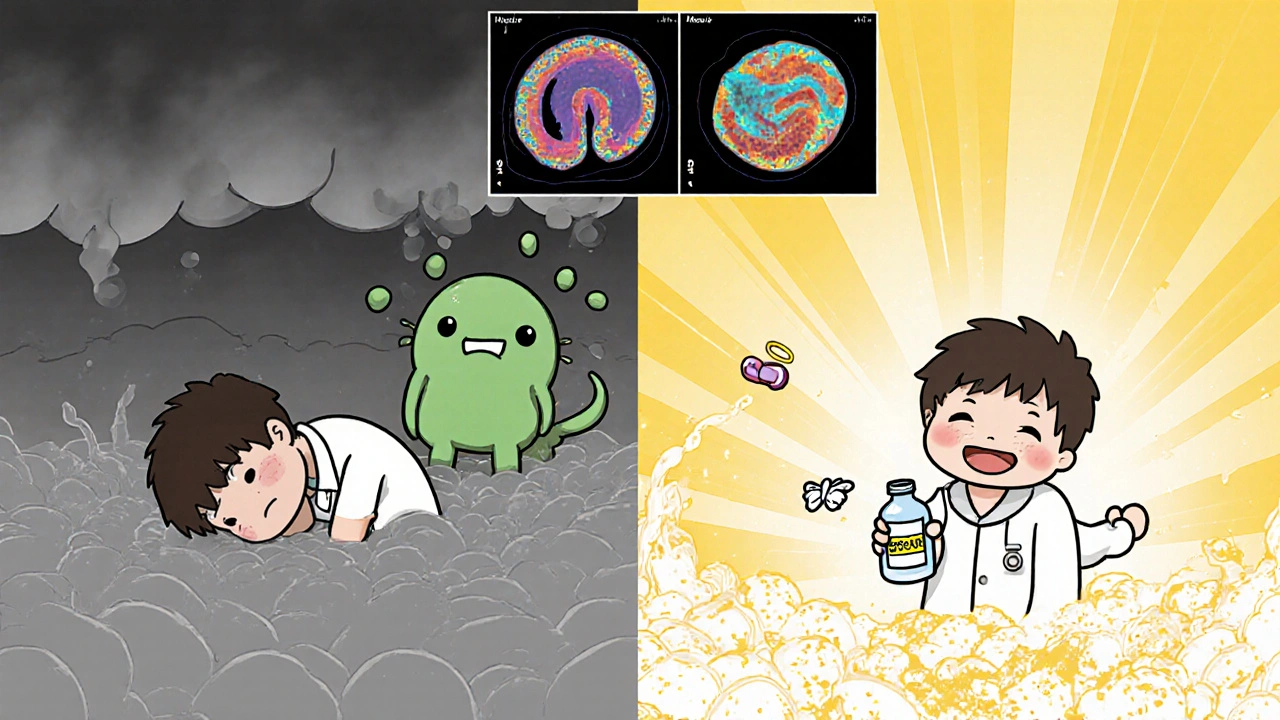
What Doesn’t Work
There’s a lot of misinformation out there.- Antibiotics alone won’t fix it. Without clearing mucus, bacteria just come back.
- Steam inhalation or herbal teas won’t clear the airways. They might feel nice, but they don’t reduce infection or improve lung function.
- Stopping smoking helps-but it won’t reverse damage. You still need active clearance.
- Exercise alone isn’t enough. But combined with airway clearance, it improves endurance and reduces fatigue.
The Bigger Picture: Access, Cost, and Future Hope
Bronchiectasis affects about 1 in 1,000 adults in the U.S.-but many more go undiagnosed. Annual costs average $18,500 per person, mostly from hospital stays and antibiotics. Medicaid patients have 3.2 times more flare-ups than those with private insurance. Why? Limited access to respiratory therapists and clearance devices. New research is promising. The Bronchiectasis Research Registry has found genetic markers that predict who’s likely to decline faster. And trials are testing inhaled bacteriophages-viruses that target only harmful bacteria-to fight antibiotic-resistant infections. For now, the best thing you can do is this: get diagnosed with a CT scan. Learn proper airway clearance from a therapist. Take antibiotics only as directed. And don’t skip the daily routine-even on days you feel okay.Frequently Asked Questions
Can bronchiectasis be cured?
No, bronchiectasis cannot be cured because the airway damage is permanent. But with consistent management-daily airway clearance, appropriate antibiotics, and hydration-progression can be slowed dramatically. Many people live full, active lives without frequent hospitalizations.
How do I know if I’m doing airway clearance right?
If you’re producing more sputum after your routine, you’re likely doing it right. You should feel lighter in the chest afterward. If you’re still coughing up the same thick mucus, or you’re not seeing improvement over 2-4 weeks, ask for a therapist re-evaluation. Most people need 3-4 sessions to learn proper technique, and 55% need a refresher within six months.
Is it safe to take azithromycin long-term?
Yes, for most people. Low-dose azithromycin (250-500mg three times a week) is well-tolerated long-term. The biggest risk is developing antibiotic resistance or hearing changes (rare). Your doctor should monitor your hearing and liver function annually. It’s not recommended if you have a history of heart rhythm problems.
Why does my sputum smell so bad?
The odor comes from bacteria breaking down proteins in the mucus, releasing sulfur compounds-similar to rotten eggs. This is common in chronic infections, especially with Pseudomonas or anaerobic bacteria. It’s a sign that mucus is trapped and infected, not just a matter of hygiene.
Can I use a humidifier instead of hypertonic saline?
No. Humidifiers add moisture to the air but don’t change the thickness of mucus inside your airways. Hypertonic saline (7% salt solution) works by drawing water into the mucus layer, thinning it so it can be cleared. Humidifiers may help with dry throat but won’t reduce infections or improve clearance.
What should I do during a flare-up?
Increase your airway clearance to twice daily. Drink at least 2 liters of water. Start your prescribed antibiotic course immediately if you have one on hand. If symptoms worsen-fever, more blood, or trouble breathing-contact your doctor. Don’t wait. Early treatment during a flare-up prevents long-term damage.
Is bronchiectasis the same as COPD or asthma?
No. COPD involves narrowed airways from smoking or pollution, while asthma is reversible airway tightening. Bronchiectasis is structural damage-airways are widened and scarred. You can have more than one, but they need different treatments. A CT scan is needed to tell them apart.






Chris Taylor
November 29, 2025Man, I didn’t realize how much I was ignoring my daily cough until I read this. I’ve been dumping out like 50mL of gunk every morning and thought it was just from smoking. Turns out I’ve had bronchiectasis for years and never got scanned. Thanks for laying it out like this.