Opioid-Induced Testosterone Deficiency (OPIAD) Assessment
This tool helps you assess whether your symptoms might be related to low testosterone caused by long-term opioid use. Note: This is not a medical diagnosis. If you have concerns, please consult a healthcare professional.
Your Assessment Result
When you’re on long-term opioids for chronic pain, you might not connect your low energy, lack of sex drive, or mood swings to the medication. But for many men, these aren’t just signs of stress or aging-they’re symptoms of something medical: opioid-induced androgen deficiency (OPIAD). It’s not rare. In fact, up to 90% of men using opioids for more than three months show low testosterone levels. Yet most doctors don’t test for it. And if you’re not tested, it’s not treated. That means millions of people are living with preventable symptoms because no one’s looking.
How Opioids Kill Your Testosterone
Your body makes testosterone through a chain reaction called the hypothalamic-pituitary-gonadal (HPG) axis. The hypothalamus sends out signals (GnRH), the pituitary responds with LH, and the testes produce testosterone. Opioids break this chain at the very start. They latch onto receptors in the hypothalamus and dull the signal. No GnRH means no LH. No LH means your testes stop making testosterone. It doesn’t matter if you’re on heroin, oxycodone, or methadone. The effect is the same. But the longer you’re on it, the worse it gets. Studies show men on opioids for over a year have testosterone levels 50-75% lower than normal. Methadone is especially harsh-average testosterone levels drop to around 245 ng/dL, well below the normal range of 300-1000 ng/dL. Even buprenorphine, often seen as a safer option, still cuts levels by about 30% compared to people not on opioids. This isn’t a side effect you can ignore. Testosterone isn’t just about sex. It’s tied to muscle, bone, mood, energy, and even heart health.What Low Testosterone Feels Like on Opioids
If you’ve been on opioids for months and feel like you’re running on empty, here’s what might be going on:- Low libido-Sex drive drops by 68-85% in affected men. This isn’t just "not in the mood." It’s a deep, persistent lack of interest.
- Erectile dysfunction-Up to 75% of men on long-term opioids struggle to get or keep an erection, even if they’ve never had issues before.
- Chronic fatigue-You’re not tired because you’re working too hard. Your body’s energy production is down. Fatigue scores in these patients are 2.5 times higher than normal.
- Mood changes-Irritability, depression, and brain fog are common. Studies show 40% higher depression symptoms compared to men with normal testosterone.
- Loss of muscle, gain of fat-You might notice your arms getting weaker, your belly getting bigger. Lean mass drops. Visceral fat increases. Bone density can fall by 15-20%, raising fracture risk.
- Anemia-Hemoglobin levels often dip to 12.3 g/dL, below the normal 14-18 g/dL. That means less oxygen in your blood, which makes fatigue worse.
Testing for OPIAD: What You Need to Ask For
If you’re on opioids long-term and have any of these symptoms, ask for a blood test. But don’t just ask for "testosterone." You need two tests:- Total testosterone-Measures all testosterone in your blood.
- Free testosterone-Measures the active, unbound portion your body can actually use.
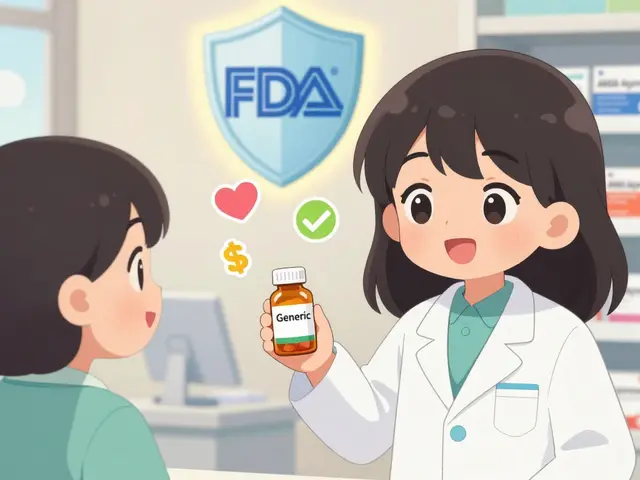
Treatment: Testosterone Replacement Therapy (TRT)
If your levels are low and symptoms match, testosterone replacement therapy (TRT) is the standard treatment. It’s not a cure for opioid dependence-but it fixes the hormone damage. Options include:- Injections-Testosterone cypionate or enanthate, 100-200 mg every 1-2 weeks. Most common, most cost-effective.
- Gels-50-100 mg daily, applied to skin. Easy to use, but you have to avoid skin contact with others for hours after.
- Patches-5-7.5 mg daily. Can cause skin irritation.
- Buccal tablets-30 mg twice daily, stuck to the gum. Less common, but avoids skin contact.
- 49% lower risk of dying from any cause
- 42% lower risk of heart attack or stroke
- 35% lower risk of hip or femur fractures
- 26% lower risk of anemia
What TRT Won’t Fix-and What It Can Hurt
TRT isn’t risk-free. The FDA requires black box warnings for testosterone therapy because of potential dangers:- Polycythemia-Red blood cell count spikes in 15-20% of users. This thickens your blood, raising stroke and clot risk.
- Lower HDL (good cholesterol)-Levels drop by 10-15 mg/dL. That’s bad for your heart.
- Acne-Happens in about 25% of gel users.
- Prostate and breast cancer-TRT is strictly forbidden if you have or are at high risk for either. PSA levels must be checked every 6 months for men over 50 or with family history.
- Testicular shrinkage-Your body stops making its own testosterone when you give it externally. That’s normal with TRT, but it’s irreversible if you stop.
What You Can Do Without Medication
If you’re not ready for TRT-or your doctor won’t prescribe it-there are natural ways to support your testosterone:- Stay lean-BMI under 25 is linked to 20-30% higher testosterone.
- Resist the weight gain-Diabetes cuts testosterone by 25-35%. Avoid sugar and processed carbs.
- Weight train-Three sessions a week of lifting can boost testosterone by 15-25%.
- Sleep 7-9 hours-Poor sleep drops testosterone by 20%. Fix your sleep schedule.
- Ditch smoking-Smokers have 15-20% lower testosterone.
- Limit alcohol-More than 14 drinks a week cuts levels by 25%.
When to Talk to a Specialist
This isn’t something your primary care doctor can handle alone. You need an endocrinologist who understands opioid-related hormone issues. Ask for a referral if:- Your testosterone is below 300 ng/dL
- You have persistent symptoms despite lifestyle changes
- You’re considering TRT
- You’ve had a fracture or anemia without clear cause
The Bigger Picture
Over 58 million people worldwide used opioids in 2022. Even if only half of them are men, that’s tens of millions at risk for OPIAD. And most don’t know it exists. This isn’t just about pain management. It’s about dignity. It’s about being able to get out of bed, have a relationship, lift your grandchild, or walk without fear of breaking a bone. Low testosterone isn’t a minor side effect. It’s a silent crisis hiding in plain sight. You don’t have to live with it. Testosterone levels can be restored. Energy can return. Mood can improve. Your body still has the capacity to heal-if you give it the right support.Can opioids cause low testosterone in women?
Yes, though it’s less studied. Women on long-term opioids can develop low estrogen and low DHEA, leading to similar symptoms like low libido, fatigue, and mood changes. Some doctors may consider DHEA supplementation, but evidence is limited. Women should also be screened for hormone imbalances if they’re on chronic opioids.
How long does it take for testosterone to recover after stopping opioids?
Recovery varies. Some men see improvement in 3-6 months after stopping opioids. Others take over a year. The longer you were on opioids, the slower the recovery. Lifestyle changes like exercise, sleep, and weight loss help speed it up. But if testosterone stays low after 6-12 months off opioids, TRT may be needed.
Is buprenorphine better than methadone for testosterone levels?
Yes. Studies show men on buprenorphine have testosterone levels about 50% higher than those on methadone. Methadone causes deeper suppression of the HPG axis. If you’re choosing between the two for opioid use disorder, buprenorphine is the better option for hormone health.
Can I take testosterone while on naloxone or naltrexone?
Yes. Naloxone and naltrexone block opioid receptors but don’t interfere with testosterone replacement therapy. TRT works independently of opioid blockade. Many men on medication-assisted treatment (MAT) safely use TRT under medical supervision.
Does testosterone therapy increase the risk of opioid relapse?
No. In fact, studies suggest the opposite. Men on TRT report improved mood, motivation, and quality of life, which can reduce the urge to self-medicate with opioids. Better hormone balance supports recovery, not relapse.
What’s the best way to monitor TRT effectiveness?
Track both symptoms and lab values. Use the ADAM questionnaire (Androgen Deficiency in Aging Males) every 3 months. Ask yourself: Is my energy up? Is my mood better? Am I getting erections again? Blood tests should show testosterone between 350-750 ng/dL, with hematocrit under 50%. If symptoms improve and labs are in range, you’re on track.




Nikhil Purohit
November 21, 2025I had no idea opioids could wreck testosterone this bad. I’ve been on oxycodone for 2 years for back pain and just assumed I was getting old or stressed. My libido’s been garbage, I’m always tired, and I’ve gained 15 lbs of belly fat despite working out. Time to ask my doc for a blood test. Thanks for laying this out.