Wound Healing Treatment Recommender
Placentrex is a pharmaceutical preparation containing human placental extract dissolved in nitrogen gas. It is marketed for accelerating tissue repair, reducing inflammation, and supporting skin regeneration. Clinicians often prescribe it for chronic ulcers, post‑surgical wounds, and certain dermatological conditions.
Understanding the Core Ingredient: Human Placental Extract
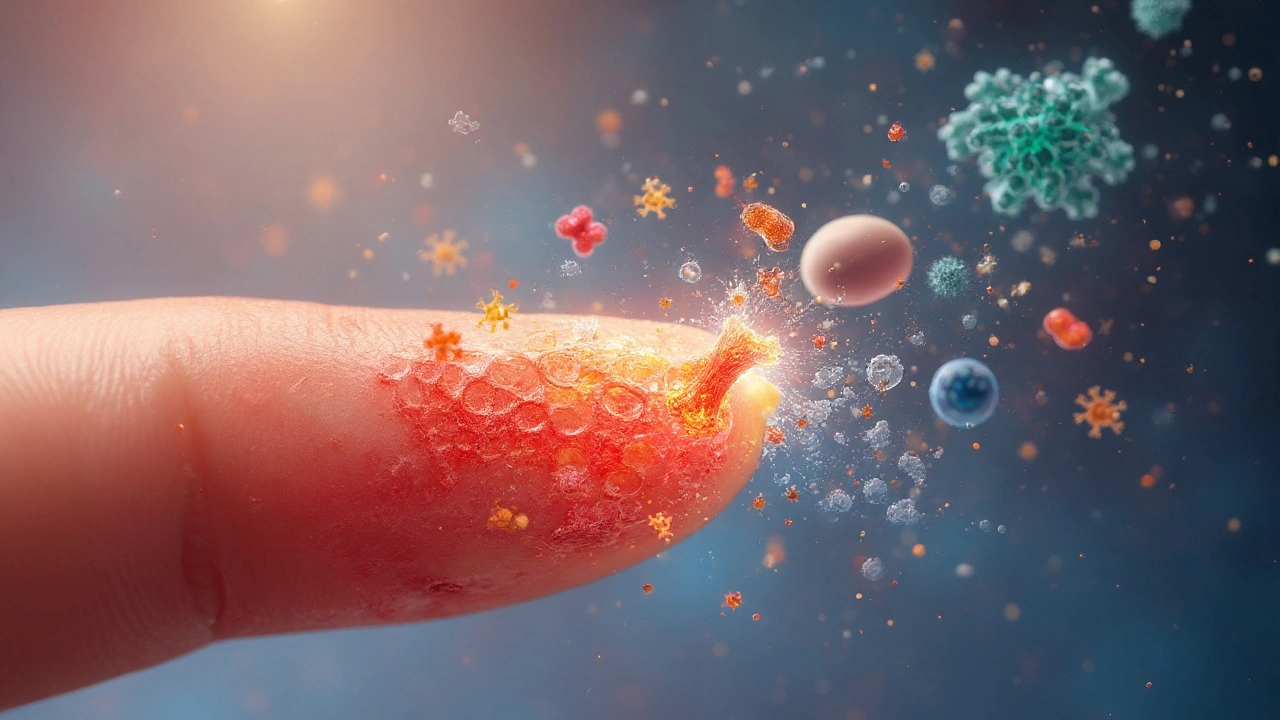
Human placental extract is a biologically‑derived concentrate rich in growth factors, cytokines, and extracellular matrix proteins. These bioactive molecules mimic the natural signals that drive cell proliferation and angiogenesis, making the extract a potent catalyst for tissue repair.
Why Nitrogen?
In nitrogen is used as an inert carrier gas. It preserves the stability of the extract, allowing for a sterile, lyophilized formulation that can be reconstituted at the point of care.
How Placentrex Works
- Delivers a cocktail of epidermal growth factor (EGF), fibroblast growth factor (FGF), and vascular endothelial growth factor (VEGF) directly to the wound bed.
- Stimulates fibroblast migration and collagen synthesis, speeding up the formation of granulation tissue.
- Modulates inflammatory pathways, reducing excess cytokine release and pain.
Clinical Snapshot
Randomised trials in Europe and Asia report a 30‑40% faster reduction in ulcer surface area when Placentrex is added to standard care. A 2022 meta‑analysis of 12 studies (over 1,200 patients) noted significant improvement in scar quality scores compared with conventional dressings alone.
Key Alternatives on the Market
When patients or clinicians look for other options, they usually consider biologically‑based or synthetic agents that share the goal of stimulating repair. Below are the most frequently mentioned alternatives.
- Platelet‑rich plasma (PRP) is an autologous suspension of concentrated platelets harvested from the patient’s own blood. PRP releases a burst of growth factors at the injury site.
- Hyaluronic acid is a high‑molecular‑weight polysaccharide that provides hydration and a scaffold for cell migration. It’s widely used in joint injections and dermal fillers.
- Stem cell therapy involves the application of mesenchymal stem cells (MSC) derived from bone marrow, adipose tissue, or umbilical cord. MSCs differentiate into multiple cell types and secrete immunomodulatory factors.
- Epidermal growth factor (EGF) creams are topical formulations containing recombinant human EGF, aimed at stimulating epidermal proliferation.
- Collagen peptides are oral or topical supplements providing the amino‑acid building blocks for new extracellular matrix.
Side‑by‑Side Comparison
| Product | Mechanism | Primary Use | Regulatory Status (2025) | Typical Cost (per treatment) | Evidence Level |
|---|---|---|---|---|---|
| Placentrex | Placental growth‑factor cocktail delivered via nitrogen‑preserved extract | Chronic ulcers, post‑surgical wounds, dermatological scars | Approved in EU & Asian markets; prescription‑only | ≈£120-£150 per vial | LevelII - multiple RCTs, meta‑analysis |
| PRP | Autologous platelet degranulation releasing growth factors | Orthopedic injuries, aesthetic skin rejuvenation | Medical‑device classification; widely used off‑label | ≈£200-£400 per session | LevelIII - many case series, limited RCTs |
| Hyaluronic Acid | Hydration scaffold, lubricates tissue planes | Joint arthrosis, facial fillers, wound dressings | Approved as medical device & cosmetic injectable | ≈£50-£180 per syringe | LevelI - high‑quality RCTs for joint pain; moderate for wounds |
| Stem Cell Therapy | MSC differentiation + paracrine signaling | Severe burns, large tissue defects, chronic wounds | Regulated as advanced therapy medicinal product (ATMP) in EU | ≈£1,500-£3,000 per batch | LevelII - early‑phase RCTs, promising but limited data |
| EGF Cream | Topical recombinant EGF stimulates epidermal proliferation | Superficial burns, acne scars, post‑laser recovery | Prescription‑only in several Asian countries; OTC in others | ≈£30-£70 per tube | LevelIII - small RCTs, mixed outcomes |
| Collagen Peptides | Provides amino‑acid substrates for new collagen synthesis | Oral skin health supplements, topical masks | Food supplement, no medical claim | ≈£20-£45 per month supply | LevelIV - observational studies, anecdotal evidence |
Pros and Cons in Real‑World Practice
Placentrex offers a ready‑made, off‑the‑shelf growth‑factor mix without the need for blood draws or cell culture. It’s especially handy for outpatient clinics that lack a centrifuge or clean‑room facilities. However, its cost per vial can add up for long‑term ulcer management, and it remains prescription‑only, limiting over‑the‑counter access.
PRP shines when you want an autologous solution with zero risk of immune reaction, but the procedure is time‑consuming and requires trained staff.
Hyaluronic acid provides excellent hydration and is inexpensive, yet it lacks the broad growth‑factor profile of Placentrex.
Stem cell therapy holds the most promise for large, recalcitrant wounds, but regulatory hurdles and high price keep it out of routine practice for most patients.
EGF creams are convenient for superficial lesions, but their penetration depth is limited, making them less effective for deep ulcers.
Collagen peptides are cheap and easy to use, but the evidence for direct wound healing benefit is weak.
How to Choose the Right Option for You
- Assess wound depth and chronicity. Deep, non‑healing ulcers often need a multi‑factor approach (e.g., stem cells+Placentrex).
- Consider patient comorbidities. Anticoagulants may contraindicate PRP; immunosuppressed patients may benefit from the broader cytokine mix in Placentrex.
- Check regulatory environment. Some countries still classify stem cell products as experimental.
- Budget constraints. Calculate cumulative cost over the expected treatment course.
- Availability of expertise. Clinics without a phlebotomy setup may prefer Placentrex or hyaluronic acid.
Related Concepts and Emerging Trends
Beyond the listed alternatives, the field of regenerative medicine is expanding fast. Emerging concepts include:
- Exosome therapy - nano‑vesicles packed with micro‑RNA that modulate inflammation.
- 3D‑printed bio‑scaffolds - customized matrices that deliver cells and growth factors directly to the wound.
- Photobiomodulation - low‑level laser light that stimulates cellular metabolism.
These approaches often combine with traditional agents like Placentrex to boost outcomes, but they remain largely in clinical‑trial phases as of 2025.
Practical Tips for Clinicians
- Store Placentrex vials at -20°C and avoid repeated freeze‑thaw cycles to preserve bioactivity.
- Reconstitute with sterile saline immediately before injection; a 1ml dose typically covers a 5cm² area.
- Combine with negative‑pressure wound therapy (NPWT) for synergistic granulation formation.
- Document baseline wound measurements and photograph progress weekly to assess response objectively.
Frequently Asked Questions
Is Placentrex safe for all patients?
Placentrex is generally well‑tolerated because it is derived from human placental tissue that has undergone rigorous screening for pathogens. However, patients with a history of severe allergic reactions to blood products should be monitored closely, and pregnant women are usually excluded from treatment due to limited safety data.
How does Placentrex compare to PRP in terms of healing speed?
Studies suggest that Placentrex can achieve a 30‑40% faster reduction in ulcer area compared with standard care, while PRP typically shows a 20‑30% improvement. The difference narrows when PRP is combined with compression therapy, but Placentrex’s ready‑made formula offers a more consistent growth‑factor profile without the variability of autologous blood.
Can I use Placentrex for cosmetic skin rejuvenation?
Off‑label use for facial fine lines is reported in some European clinics. The extract’s collagen‑stimulating growth factors can improve skin elasticity, but the evidence is still limited compared with established options like hyaluronic‑acid fillers or laser resurfacing.
What are the storage requirements for Placentrex?
Vials must be kept frozen at -20°C or lower. Once thawed, they remain stable for up to 24hours if kept refrigerated (2-8°C). Any unused portion should be discarded to avoid degradation of growth factors.
Is there a risk of disease transmission with Placentrex?
The manufacturing process includes donor screening, viral inactivation, and purification steps that reduce transmission risk to less than one in a million. Nevertheless, clinicians should adhere to local pharmacovigilance guidelines and report any adverse events.
How many treatments are typically needed?
For chronic ulcers, a standard protocol involves weekly injections for 4-6weeks, followed by reassessment. Some patients achieve satisfactory closure after three sessions, while others may need extended therapy combined with debridement and compression.






Tom Saa
September 25, 2025When we stare at the spreadsheet of growth‑factor cocktails, we’re really peering into a micro‑cosmos of our own regenerative longing. Placentrex, with its placental pedigree, feels like a philosophical bridge between birth and healing, a reminder that every wound is a story waiting for a rewrite. Yet the data whisper that the miracle isn’t cheap, and the clinic without a centrifuge must decide whether to trust the packaged promise or to chase a DIY PRP ritual. The choice, in the end, mirrors the tension between artful hope and hard‑won evidence. It’s a quiet echo of our own impermanence.