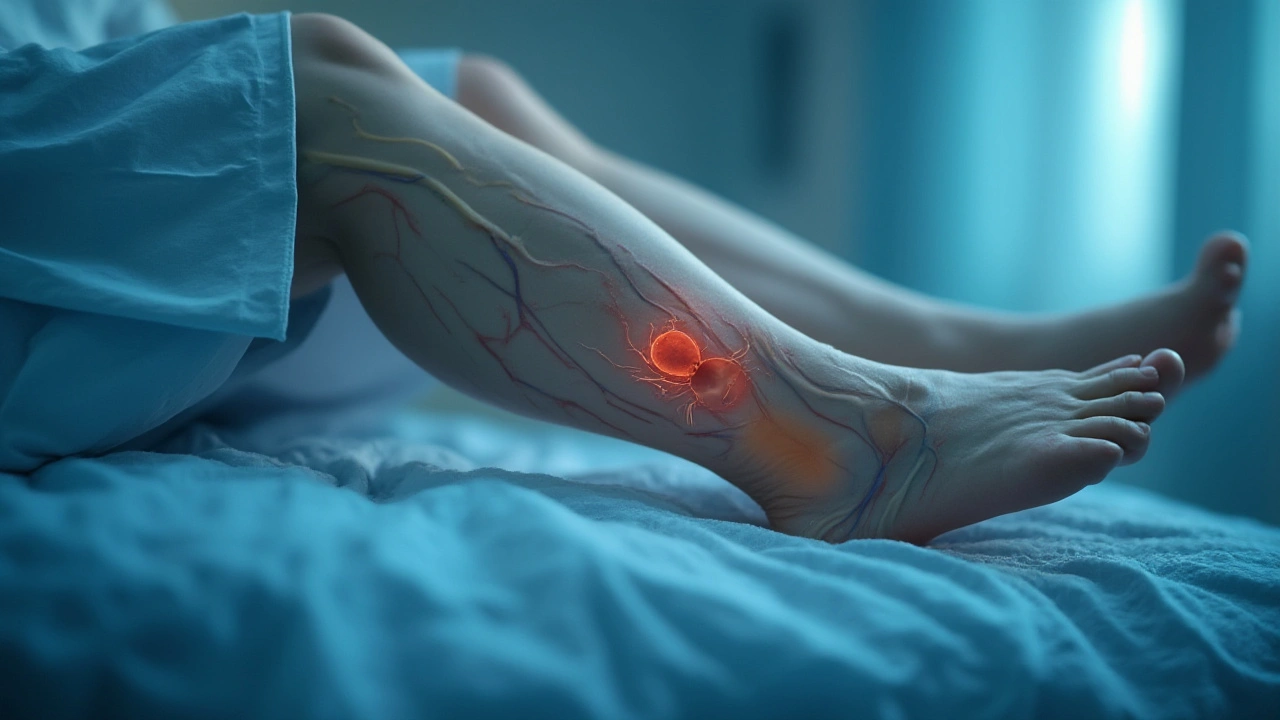
Imagine waking up after surgery, relieved it's over, only to hear the word "thrombosis." Just the thought of a blood clot freaks people out—and for good reason. They’re sneaky and can cause big trouble, from swollen legs to life-threatening lung problems. Tons of patients lie in pre-op worrying: does anesthesia itself set the stage for dangerous clots, or are there other villains hiding in the OR? Let’s roll up our sleeves and dig into what actually raises your risk, what’s just hospital legend, and what you can do to keep those veins healthy.
How Blood Clots Form During and After Surgery
The human body isn’t a fan of lying still for long stretches—the blood stagnates, and that’s when clots start hatching. Surgeons call these deep vein thromboses (DVTs), and they often lurk in the legs after long operations. But here’s something wild: the risk starts building from the moment you stop moving, not from a mysterious "clotting drug" in the anesthesia.
Any kind of surgery, especially knee replacements, hip operations, or even some long abdominal procedures, makes your blood more likely to form a clot. Why? Well, first there’s the fact that you’re not moving. Muscle contractions help push blood through your veins, so when you’re flat on your back for hours, blood slows down, and that’s a paradise for clot formation. Add to that surgical injury—cutting and sewing tissues pokes the body into repair mode, which naturally speeds up clotting to prevent bleeding. It’s a survival thing, just sometimes too effective.
- Major joint surgeries like total knee or hip replacements have the highest clot risk, with some studies showing DVT rates as high as 40% without preventive treatment.
- Simple day surgeries (think wisdom teeth or mole removal) don’t have the same risk, since you’re not immobile for hours and usually jump up right after.
Check out this quick look at surgery types and their relative risks in the table below:
| Surgery Type | Typical Clot Risk (No Prevention) |
|---|---|
| Hip Replacement | 30-60% |
| Knee Replacement | 40-70% |
| Major Abdominal Surgery | 15-30% |
| Laparoscopic Cholecystectomy (gallbladder removal) | 2-5% |
| Minor Outpatient Surgery | <1% |
The more you know about your kind of procedure, the better prepared you’ll be to ask your surgeon or anesthesiologist real questions about your own risk. But does the anesthesia itself—gas, IV medications, those mysterious cocktail bags—flip the switch for clots? Let’s clear up the facts.
Does Anesthesia Directly Cause Blood Clots?
This one’s at the heart of the debate. Patients worry that being "put under" somehow thickens their blood, raising their chance for a DVT. But current research points in a different direction. Anesthesia—either general (where you’re totally out) or regional (like spinal or epidural)—isn’t the main driver for clot formation. It’s more about what anesthesia does: keeping you still and pain-free during a procedure, which means hours without movement and a natural dip in blood flow.
Here’s what the science says:
- General anesthesia can slightly affect blood vessel contraction and heart function, but it doesn’t directly make your body form more clots.
- Spinal or epidural anesthesia actually seems to be a little safer—patients often move their legs sooner and experience less blood stagnation than those who’ve had general anesthesia.
- Most studies pin the bulk of clot risk on surgical trauma (meaning cuts, stitches, and internal healing), not anesthesia alone.
- Risk also climbs the longer you’re under—more time without movement means more time blood can pool in the veins.
Some folks have extra risk factors that anesthesia can’t control. For example, a smoker, someone taking birth control pills, or a person with a family history of blood clots: all of these things create stickier blood. Add in obesity, cancer, or being over 60, and your risk bumps up again.
Want deeper details? I found this solid rundown that busts some myths about anesthesia and surgery: does anesthesia cause blood clots. It lays out why post-op complications usually trace back to immobility and the body's healing response.
Of course, the story changes a little if you’re looking at massive trauma or operations for cancer, which can turbocharge the clotting system. But it’s still the surgical process—and the days of reduced mobility afterward—that crank up the biggest danger signs. So, the question shouldn’t be "Will anesthesia cause me to clot?" Instead, ask: "What steps can I and my care team take to lower my post-op clot risk?" That’s where prevention comes in.

Practical Ways to Beat Blood Clots After Surgery
Stopping clots before they start is all about movement, awareness, and sometimes a little preventive medicine. Hospitals these days are obsessed with getting people out of bed right after surgery—sometimes even within a few hours. It might feel awkward wobbling around on fresh stitches, but every footstep gets your blood moving and slashes DVT odds big time.
Doctors might give you elastic compression stockings or inflatable boots that squeeze your legs in the hospital bed. These fancy sleeves mimic muscle contractions when you can’t walk, which helps keep that blood flowing. In some high-risk cases, blood thinners are the gold standard, especially for orthopedic surgeries. You might get a quick daily shot or a pill for a few days or weeks after you leave the hospital.
- If you’re stuck in bed, do these: flex your feet up and down often, pump your calves, and move your toes every hour.
- If you had regional anesthesia, ask if you can start gentle leg movement sooner.
- Hydrate like you mean it—dehydration makes blood thicker and slower, which is basically inviting clots for a sleepover.
- Stick to your blood thinner schedule if your team prescribed one. Skipping even one dose raises the threat level.
- Keep an eye out for symptoms after you’re home: calf swelling, pain, unusual warmth, or redness. Shortness of breath and chest pain need an ER visit, not a Google search.
Here’s a roll-up of some clever ways hospitals and patients work together:
| Prevention Method | Best For | How It Helps |
|---|---|---|
| Compression Stockings/Boots | Most surgical patients | Improves blood flow in legs |
| Blood Thinners | High-risk patients (joint replacements, cancer surgeries) | Prevents clots from growing |
| Early Ambulation | Almost everyone post-surgery | Restores muscle-pumping action |
| Hydration | All patients | Keeps blood from thickening |
Even people with zero known risk sometimes get unlucky, so don’t be shy about talking directly to your surgical team about your history, prior clots, or medications. And don’t be that person who shrugs off thigh cramps or weird swelling, assuming it’ll go away. Catching a DVT early can mean the difference between a short course of blood thinners and a dangerous ride with a pulmonary embolism.
If you want to be proactive, plan your recovery. Ask about physical therapy options, at-home movement routines, or follow-up appointments for DVT screening. Bring your questions, share your worries, and remember: the more you know, the safer you’ll feel stepping into (and out of) the operating room. And for that burning question—can anesthesia really make me clot?—the evidence just doesn’t back up the scare stories. It’s *immobility* and your body’s healing response that are the main plot-twisters in this medical mystery.
The OR doesn’t have to feel like a lottery. With smart planning, watchful recovery, and a dose of solid info, you can steer clear of surgical blood clots and get back on your feet a whole lot faster.







Leah Beazy
July 24, 2025Just had knee surgery last month and honestly? The compression boots felt like a weird alien massage but they worked. Got up and shuffled the next day and my leg didn’t turn into a brick. Do the damn foot pumps.
Also hydration is non-negotiable. I drank water like it was my job.