Ever taken a pill and wondered if your breakfast ruined it? Or skipped a dose because you didn’t eat breakfast and weren’t sure if it was safe? You’re not alone. Millions of people take medications every day without realizing that what’s on their plate can make the difference between a drug working as it should - or not working at all.
Food doesn’t just fill your stomach. It changes how your body handles medicine. Some drugs work better with food. Others are ruined by it. And timing? That’s not just a suggestion. It’s science.
Why Food Changes How Medicines Work
Your digestive system isn’t just a pipe for food. It’s a complex chemical factory. When you eat, your stomach slows down, your bile flows, your pH shifts, and your gut starts absorbing nutrients. All of that affects drugs.
High-fat meals, for example, can delay gastric emptying by up to two hours. That means a pill you swallowed at 7 a.m. might not even reach your small intestine - where most drugs are absorbed - until 9 a.m. or later. For some medications, that delay doesn’t matter. For others, it’s a disaster.
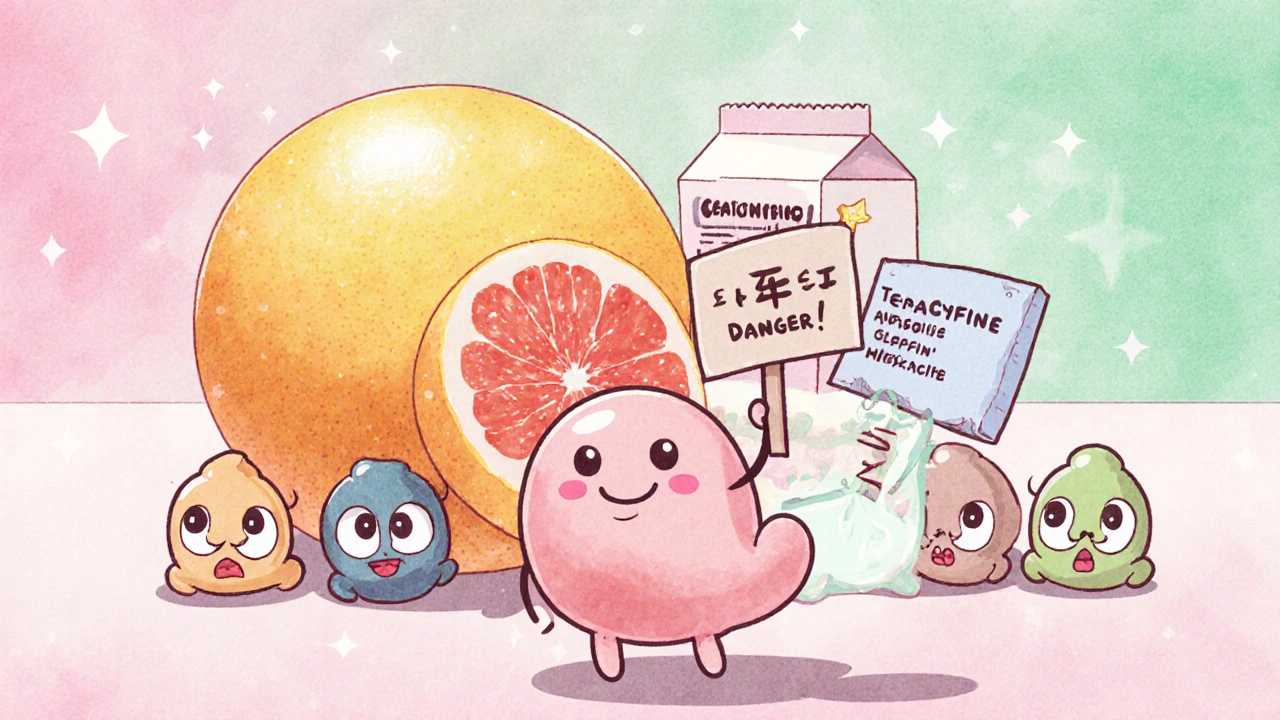
Then there’s the chemistry. Calcium in milk binds to antibiotics like tetracycline, trapping them so your body can’t absorb them. Fat helps dissolve drugs like griseofulvin, making them 200-300% more effective. Acidic stomach conditions help itraconazole absorb - but high-fat meals raise stomach pH, lowering absorption by 40%.
These aren’t rare cases. The FDA says 35% of new drugs approved between 2015 and 2022 came with specific food-effect instructions. That’s not an accident. It’s a requirement.
When to Take Medications on an Empty Stomach
Some drugs need your stomach to be completely empty. That means no food - not even a cracker - for at least one hour before and two hours after taking them.
Levothyroxine, the most common thyroid medication, is one of the most sensitive. Food can cut absorption by 30-55%. That means you could be taking your full dose, but your body only gets half of it. Result? Fatigue, weight gain, brain fog - symptoms that look like your thyroid isn’t under control, even when you’re dosing correctly.
Other medications that require an empty stomach:
- Alendronate (for osteoporosis) - food blocks absorption completely
- Levothyroxine - must be taken with plain water only, no coffee, no juice
- Amoxicillin (in some formulations) - food reduces peak levels by up to 40%
- Carbidopa/levodopa (for Parkinson’s) - protein in food competes with absorption
The rule is simple: take these first thing in the morning, before breakfast. Set an alarm. Drink a full glass of water. Wait 30-60 minutes before eating. If you forget, wait until your next meal - but don’t take it with food.
When Food Helps Your Medicine Work Better
Not all drugs hate food. Some actually need it.
Nitrofurantoin, an antibiotic for urinary tract infections, absorbs 40% better with food. That’s not a small boost - it’s the difference between clearing the infection and letting it linger.
Cefpodoxime, another antibiotic, sees a 50-60% increase in absorption when taken with a meal. Same with griseofulvin, the antifungal for nail infections. Take it on an empty stomach, and it barely works. Take it with a fatty meal - like eggs and avocado - and it works as intended.
Sulfonylureas like glipizide and glyburide are diabetes drugs that stimulate insulin release. Take them on an empty stomach, and your blood sugar can crash - fast. The American Diabetes Association reports that 23% of patients who skip meals with these drugs end up with symptoms of hypoglycemia: shaking, sweating, confusion, even fainting. The fix? Take them 30 minutes before eating. That way, the drug kicks in just as your blood sugar starts rising from food.
And then there’s semaglutide (Ozempic, Wegovy). Novo Nordisk’s own data shows that taking it within 30 minutes of eating reduces absorption by 44%. That’s why the label says: wait at least 30 minutes after your last bite.
What Counts as ‘With Food’?
Here’s where people get confused. ‘Take with food’ doesn’t mean ‘take with a full meal.’
For many drugs - especially those that cause stomach upset like ibuprofen or naproxen - a small snack is enough. A few crackers, a banana, a slice of toast. That’s all it takes to protect your stomach lining without blocking absorption.
But for others - like some HIV medications - you need at least 200-300 calories. A handful of nuts or a yogurt won’t cut it. You need a proper snack: peanut butter on toast, a protein bar, or a small sandwich.
A 2023 Express Scripts report found that 45% of patients misunderstand this. One woman took her antiretroviral with a cup of coffee and a biscuit - thinking that was ‘with food.’ The drug didn’t absorb. Her viral load spiked. She didn’t realize why until her pharmacist asked what she ate.
So if your prescription says ‘take with food,’ ask: ‘What kind of food?’
What to Avoid: The Big Culprits
Some foods are notorious for messing with meds - and most people don’t know it.
- Dairy products - milk, cheese, yogurt - bind to tetracycline, doxycycline, and ciprofloxacin. Don’t take them within two hours of these antibiotics.
- Grapefruit juice - blocks enzymes in your gut that break down over 85 drugs, including statins, blood pressure meds, and some antidepressants. One glass can cause dangerous drug buildup for days.
- Leafy greens - high in vitamin K, which interferes with warfarin (Coumadin). You don’t need to avoid spinach - just keep your intake consistent. A salad every day? Fine. A salad one day and none the next? That’s a problem.
- Alcohol - worsens liver stress with acetaminophen, increases drowsiness with benzodiazepines, and spikes blood pressure with MAO inhibitors.
These aren’t myths. They’re documented in FDA labeling, clinical trials, and pharmacy databases. Grapefruit juice alone has been linked to over 85 drug interactions - some fatal.
How to Get It Right: Practical Tips
Here’s how real people make this work:
- Use a pill organizer with time slots - label each slot: ‘AM: empty stomach,’ ‘PM: with dinner.’
- Set phone alarms - one for when to take the pill, one for when to eat.
- Keep a simple log - write down what you ate and when you took your meds. You’ll spot patterns.
- Ask your pharmacist - they’re trained for this. Don’t assume your doctor explained it clearly.
- Use apps like Medisafe - they send reminders with food instructions. Users report 27% fewer timing errors.
For elderly patients on five or more medications, this isn’t optional. A 2022 study in the Journal of the American Geriatrics Society found they’re 65% more likely to have dangerous interactions. One pill, taken 20 minutes after a bowl of oatmeal with milk, could be the difference between staying out of the hospital - or not.
Why This Matters More Than You Think
Food-drug interactions aren’t just about side effects. They’re about cost, hospital visits, and even death.
The U.S. spends over $500 billion a year on medication-related problems. About 8% of that - roughly $40 billion - comes from food interactions. That’s not just wasted money. It’s lost time, pain, and health.
And it’s preventable.
When patients get clear, personalized instructions - not just a label that says ‘take with food’ - adherence improves by 35%. That’s not a small number. That’s life-changing.
Emerging tech is helping too. Ingestible sensors that track stomach pH and emptying time are now in clinical trials. One 2023 study showed a 38% improvement in drug absorption when timing was adjusted in real time based on your body’s response - not a generic rule.
But you don’t need a sensor. You just need to know your meds.
Final Rule: Consistency Beats Perfection
The Australian Prescriber says it best: ‘For most medicines, especially those used for chronic conditions, a delay in the onset of absorption is of no clinical consequence as long as the amount of drug absorbed is unaffected.’
That’s the key. You don’t need to be a scientist. You just need to be consistent.
If you take your blood pressure pill with breakfast every day - even if it’s not perfectly timed - your body adapts. That’s better than taking it on an empty stomach one day, with a big lunch the next, and skipping it entirely on weekends.
But for the 25% of medications that really need precision - thyroid meds, antibiotics, diabetes drugs, antivirals - timing isn’t a suggestion. It’s the treatment.
Know your pills. Know your meals. And when in doubt - ask. Your body will thank you.
Can I take my medication with coffee?
Coffee can interfere with some medications. It slows the absorption of thyroid meds like levothyroxine and can reduce the effectiveness of certain antibiotics. For most drugs, wait at least 30-60 minutes after taking your pill before drinking coffee. If you’re unsure, check your medication label or ask your pharmacist.
What if I forget to take my pill on an empty stomach?
If you took a medication that needs an empty stomach with food, don’t double up. Wait until your next scheduled dose. Taking extra can be dangerous. Instead, adjust your routine: set an alarm to take it first thing in the morning, before anything else. For drugs like levothyroxine, consistency matters more than perfection.
Do I need to avoid all dairy with antibiotics?
Only with certain antibiotics: tetracycline, doxycycline, ciprofloxacin, and some others. These bind to calcium in milk, yogurt, and cheese, blocking absorption. Wait at least two hours after taking the antibiotic before consuming dairy. Other antibiotics, like amoxicillin, aren’t affected.
Is grapefruit juice really that dangerous with meds?
Yes. Grapefruit juice blocks enzymes that break down over 85 medications, including statins, blood pressure drugs, and some anti-anxiety pills. Even a small glass can cause dangerous drug buildup in your blood for days. If you take any prescription meds, avoid grapefruit entirely - or check with your doctor or pharmacist.
Can I take my meds with water instead of food?
Water is fine - and often required - for medications that need an empty stomach. But if your pill says ‘take with food,’ water alone won’t help. You need calories. A small snack like a banana, a few crackers, or a spoonful of peanut butter is enough for most drugs. The goal is to coat your stomach and aid absorption - not just swallow the pill.
Why do some meds need to be taken before meals and others after?
It depends on how the drug works. Drugs like glipizide (for diabetes) need to be taken 30 minutes before eating so they start working as your blood sugar rises. Others, like NSAIDs, are taken with food to protect your stomach. Some, like antibiotics, are taken with food to improve absorption. Always follow the label - the timing is based on how your body absorbs the drug.
If you take multiple medications, keep a printed list with food instructions next to your pill organizer. Review it every month. Ask your pharmacist to walk you through each one. This isn’t just about taking pills - it’s about making sure they work.





Matthew Peters
November 20, 2025So let me get this straight - I’ve been taking my amoxicillin with peanut butter for years because it tasted better, and now you’re telling me it might’ve been useless the whole time? 😅