When you stand up from a chair, your body automatically adjusts your blood pressure so you don’t faint. Your heart beats faster, your blood vessels tighten, and your brain gets the oxygen it needs. But if you have autonomic neuropathy, that automatic system breaks down. You might feel dizzy, see spots, or even pass out within seconds. At the same time, your stomach might refuse to empty, leaving you bloated, nauseous, or vomiting after meals. These aren’t random side effects-they’re direct signs of nerve damage in your autonomic nervous system.
What Autonomic Neuropathy Actually Does
Autonomic neuropathy isn’t just "nerve damage." It’s the failure of the part of your nervous system that runs your body in the background-heart rate, digestion, sweating, blood pressure, even bladder control. Unlike the nerves that let you move your fingers or feel a pinprick, these autonomic nerves don’t send signals you can consciously control. When they’re damaged, your body loses its ability to respond to basic changes like standing up, eating, or getting hot.
Most cases-85% to 90%-come from long-term diabetes. High blood sugar slowly chokes off the tiny blood vessels that feed these nerves. But it’s not just diabetes. Autoimmune disorders, certain chemotherapy drugs like vincristine, Parkinson’s disease, and even some viral infections can trigger it. The problem? Most people don’t realize they have it until symptoms become severe. A 2021 study found that primary care doctors miss the diagnosis in 70% of cases. By then, the nerves are already significantly damaged.
Why Your Blood Pressure Plummets When You Stand
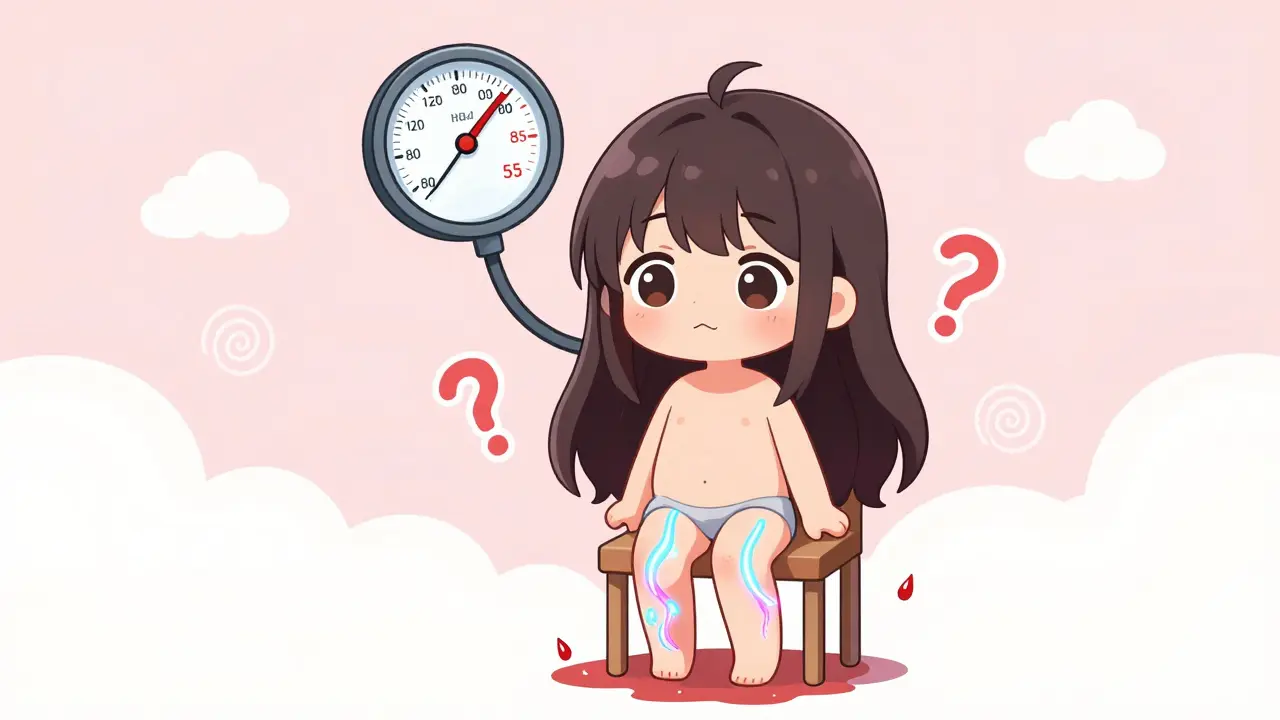
Standing up should trigger a reflex: your blood vessels constrict, your heart pumps harder, and your blood pressure stays steady. In autonomic neuropathy, that reflex is broken. The nerves that tell your blood vessels to tighten don’t send the signal. So when you stand, blood pools in your legs and abdomen, and your brain gets less blood. That’s orthostatic hypotension.
Doctors define it as a drop of at least 20 mmHg in systolic pressure (the top number) or 10 mmHg in diastolic (the bottom number) within three minutes of standing. But in real life, it’s often worse. Studies show people with severe autonomic neuropathy can drop 35 mmHg or more. Some patients go from 120/80 to 85/55 in under 30 seconds. That’s not just dizziness-it’s blackouts, falls, and hospital visits.
Not everyone drops blood pressure. Some develop POTS-Postural Orthostatic Tachycardia Syndrome. Instead of low pressure, their heart races. Their heart rate jumps more than 30 beats per minute when standing, even if blood pressure stays normal. This affects mostly young women and can be just as disabling. One patient described it as "feeling like my heart was trying to escape my chest every time I walked to the kitchen."
Doctors test for this with a simple 10-minute active stand test. They measure your blood pressure and heart rate while you’re lying down, then again after you stand. If your systolic pressure drops 20 mmHg or more, it’s a red flag. Heart rate variability testing during deep breathing is another key tool-if your heart doesn’t speed up when you inhale and slow down when you exhale, your autonomic nerves are impaired.
What’s Going On Inside Your Gut
While blood pressure drops get attention, gastrointestinal problems are just as common-and often more frustrating. Up to 55% of people with autonomic neuropathy have GI symptoms. The most well-known is gastroparesis: your stomach doesn’t empty properly. Food sits there for hours, fermenting, causing bloating, nausea, and vomiting. A 2019 study found that 78% of gastroparesis patients with autonomic neuropathy vomited at night. Some vomit multiple times a day.
It’s not just the stomach. The whole digestive tract slows down. Constipation affects 60% of patients, with bowel movements dropping to just 1.2 per week-far below the normal 4-5. Others get diarrhea, often at night. Many alternate between constipation and diarrhea, which makes it hard to pin down the cause. This isn’t IBS. It’s nerve damage.
Why does this happen? The nerves controlling gut muscle contractions are damaged. Food doesn’t move. Bacteria overgrow in the small intestine-called SIBO-because the normal sweeping motion (called the migrating motor complex) stops. A 2021 study found that 52% of autonomic neuropathy patients with GI symptoms had SIBO, compared to only 15% of healthy people. That’s why bloating, gas, and diarrhea persist even on a "clean" diet.
Esophageal problems are also common. Swallowing becomes difficult because the muscles don’t contract right. This can lead to food getting stuck, choking, or even aspiration pneumonia if food enters the lungs.

How Doctors Diagnose It
There’s no single blood test for autonomic neuropathy. Diagnosis relies on symptoms, physical tests, and specialized tools.
- Active stand test: Measures blood pressure and heart rate changes when standing. A drop of 20 mmHg systolic or 10 mmHg diastolic confirms orthostatic hypotension.
- Heart rate variability: You breathe deeply for one minute. If your heart rate doesn’t change enough between inhaling and exhaling, your autonomic nerves are impaired.
- Valsalva maneuver: You blow into a tube to create pressure. If your heart rate and blood pressure don’t respond normally, it’s a sign of nerve damage.
- Gastric emptying scintigraphy: You eat a meal with a tiny radioactive tracer. A camera tracks how fast it leaves your stomach. If more than 10% remains after 4 hours, you have gastroparesis.
- COMPASS-31 questionnaire: A 31-question survey that scores autonomic symptoms from 0 to 100. A score above 30 means significant dysfunction.
Many patients wait years for a diagnosis. One study found the average time from first symptom to confirmed diagnosis is 4.7 years. By then, nerve damage is often advanced. That’s why experts now recommend that all diabetics with more than 7 years of disease get screened annually with a simple 3-minute stand test.
Treatment: What Actually Works
Treatment isn’t about curing autonomic neuropathy-it’s about managing symptoms and preventing complications.
For Blood Pressure Drops
- Compression stockings: Wearing 30-40 mmHg compression socks helps push blood back up from your legs. Studies show they reduce orthostatic symptoms by 35%.
- Abdominal compression garments: These are like tight belts worn around the belly. They prevent blood from pooling in the abdomen. One 2022 trial showed a 40% reduction in dizziness and fainting.
- Fludrocortisone: This drug makes your body hold onto salt and water, increasing blood volume. It helps 60% of patients, but 35% develop high blood pressure when lying down-so timing matters.
- Midodrine: This tightens blood vessels. It works for 70% of people, but you have to take it 3-4 times a day and avoid lying down for hours after. Otherwise, you risk dangerous supine hypertension.
- Ivabradine: For POTS patients with fast heart rates, this drug slows the heart without lowering blood pressure. It reduces heart rate by 15-25 bpm in 65% of users.
For GI Symptoms
- Diet changes: Eat 6 small meals a day instead of 3 big ones. Avoid high-fat and high-fiber foods-they slow digestion. A low-fat, low-residue diet improved symptoms in 60% of patients.
- Pyridostigmine: This drug improves nerve signals to the stomach. It’s now recommended as a first-line treatment for diabetic gastroparesis, with 55% of patients reporting symptom improvement and fewer side effects than older drugs.
- Erythromycin: An antibiotic that also stimulates stomach contractions. It works well short-term, but most people develop tolerance within 2-4 weeks.
- Metoclopramide: Used to be a go-to, but it carries a black box warning for irreversible movement disorders after 12 weeks. Most doctors now avoid it unless absolutely necessary.
- Fecal microbiota transplantation (FMT): Early trials show promise. In a 2023 NIH study, FMT improved GI symptoms in 40% of patients after six months by resetting gut bacteria.

Life With Autonomic Neuropathy
It’s not just medical-it’s lifestyle. Patients report avoiding hot showers, standing for long periods, or eating large meals before social events. Many wear compression gear daily. Salt intake often increases to help blood pressure. One Reddit user wrote: "I keep a water bottle and salt packets in my purse. If I feel dizzy, I chug water and eat salt. It’s not glamorous, but it keeps me upright."
Work becomes harder. A 2023 study found 78% of severe cases had to quit or reduce work hours. Brain fog during blood pressure drops makes focus impossible. Social life shrinks-55% avoid restaurants because they can’t predict when they’ll vomit or feel sick.
But there’s hope. New biomarkers like neurofilament light chain in the blood may soon allow earlier diagnosis before symptoms start. The American Diabetes Association will soon recommend annual screening for all long-term diabetics. And with better drugs like pyridostigmine and non-drug tools like compression garments, many patients are regaining control.
The key is recognizing these symptoms early. If you have diabetes and you’re dizzy when you stand, or you’re vomiting after meals, don’t brush it off as "just aging" or "stress." Ask your doctor about autonomic neuropathy. The sooner you start managing it, the more of your life you keep.
Can autonomic neuropathy be reversed?
In most cases, nerve damage from autonomic neuropathy cannot be fully reversed. However, early diagnosis and strict blood sugar control in diabetic patients can stop or slow further damage. Some mild symptoms, especially in non-diabetic cases, may improve with treatment. The goal is management-not cure.
Is orthostatic hypotension the same as POTS?
No. Orthostatic hypotension means your blood pressure drops too much when standing. POTS means your heart rate spikes too much, but your blood pressure stays normal. Both are caused by autonomic nerve damage, but they affect different parts of the system. Some people have both.
Why do I feel dizzy even when I’m not standing?
Autonomic neuropathy can cause blood pressure to drop even while sitting or lying down, especially after eating, in heat, or during stress. Your body can’t adjust properly. This is called non-orthostatic hypotension and is common in advanced cases.
Can diet really help with gastroparesis?
Yes. A low-fat, low-fiber diet with small, frequent meals improves symptoms in 60% of patients. Fat and fiber slow stomach emptying, so reducing them helps food move more predictably. Avoiding carbonated drinks and lying down after eating also helps.
How do I know if I should see a specialist?
If you have diabetes and experience frequent dizziness when standing, unexplained vomiting, chronic constipation or diarrhea, or fainting spells, ask your doctor for a referral to a neurologist or autonomic specialist. Don’t wait-early intervention can prevent serious complications like falls, malnutrition, or heart problems.
What’s Next?
Research is moving fast. Blood tests that measure nerve damage through neurofilament light chain could diagnose autonomic neuropathy before symptoms appear. New drugs are in trials. Fecal transplants are being tested to fix gut bacteria linked to GI symptoms. The American College of Cardiology may soon lower the threshold for diagnosing orthostatic hypotension from 20 mmHg to 15 mmHg-meaning more people will be caught early.
But the biggest gap isn’t technology-it’s awareness. Most people don’t know autonomic neuropathy exists. Many doctors still think it’s just "diabetic complications" and don’t test for it. If you’re living with unexplained dizziness, GI issues, or heart rate swings, you’re not alone. And you don’t have to suffer in silence. Ask the right questions. Get tested. Take control-because your body’s automatic systems still deserve to work.




Alexandra Enns
January 24, 2026Okay but let’s be real-this whole thing is just Big Pharma’s way to sell you compression socks and $800 pills. They don’t want you to know that standing up too fast is just your body saying "I’m tired of your sugar addiction." Stop buying into the medical industrial complex and start drinking salt water and walking barefoot on grass. I’ve cured my own neuropathy with lemon juice and quantum healing. 🤷♀️