Managing pain after giving birth is hard enough - but when you’re also breastfeeding, every medication decision feels heavier. You don’t want to suffer, but you also don’t want to risk your baby’s health. The good news? Most pain medications are safe while breastfeeding. The bad news? Some are dangerously risky, and not everyone knows which ones. This isn’t about fear. It’s about knowing what works, what doesn’t, and how to use it right.
What Pain Medications Are Safe While Breastfeeding?
The two safest, most recommended options for postpartum pain are ibuprofen and acetaminophen. These aren’t just "probably okay" - they’re backed by decades of research and endorsed by the American College of Obstetricians and Gynecologists (ACOG), the Academy of Breastfeeding Medicine, and the FDA.
Ibuprofen transfers into breast milk at only 0.6-0.7% of the maternal dose. Peak levels hit your milk about 1-2 hours after you take it, then drop fast. That means you can take it right after nursing, and by the next feeding, levels in your milk are low. Acetaminophen is even simpler: only 0.1-1.0% makes it into breast milk, and it clears out within a few hours. Neither affects your milk supply. Neither causes drowsiness or breathing issues in babies.
For most women, alternating these two every 3 hours gives steady pain control without overloading your system. For example: acetaminophen at 8 a.m., ibuprofen at 11 a.m., acetaminophen at 2 p.m., and so on. This keeps pain managed while minimizing total medication exposure.
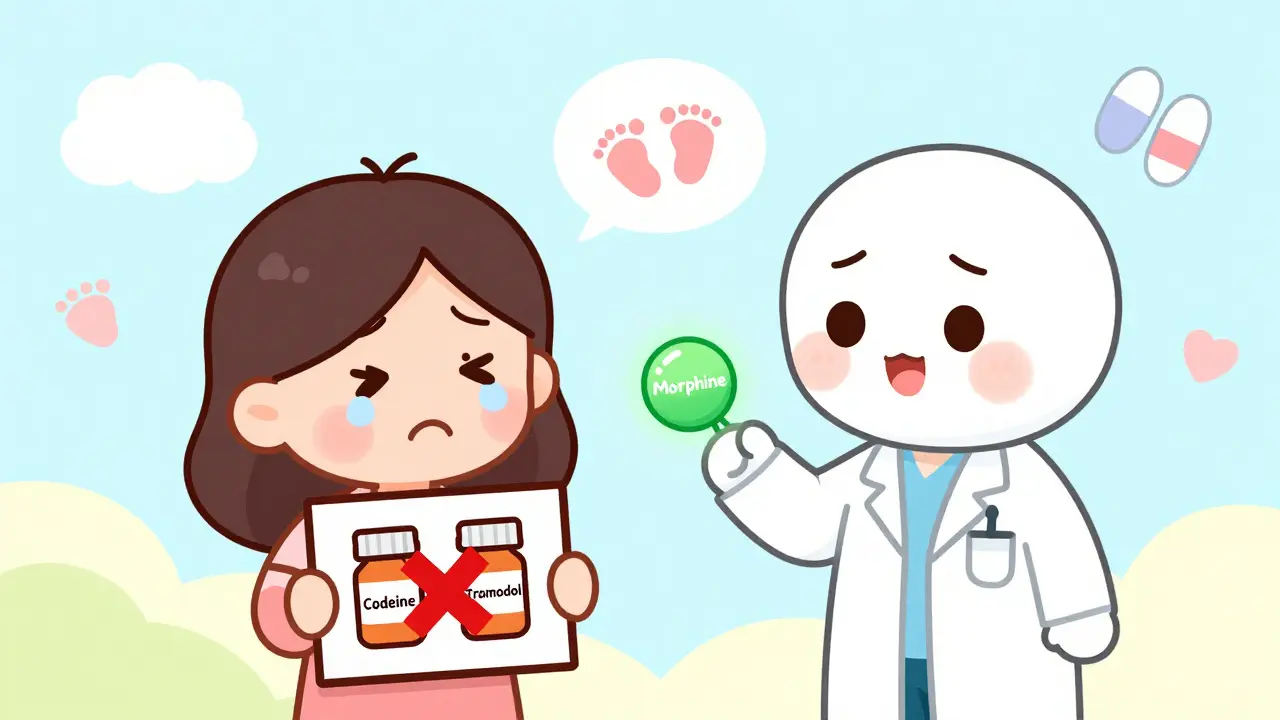
Why Codeine and Tramadol Are Dangerous - Even in Small Doses
Some doctors still prescribe codeine or tramadol after birth because they’re strong. But they’re not safe for breastfeeding mothers. In 2017, the FDA issued a strong warning: do not use codeine while breastfeeding. In 2018, they added tramadol to that list. Why? Because of something called ultra-rapid metabolism.
About 1 in 100 white women (and fewer in other groups) have a genetic variation that turns codeine into morphine too fast. Tramadol turns into M1, a powerful opioid metabolite, at unpredictable rates. You can’t test for this before taking the drug. You won’t know you’re one of them until your baby gets sick.
Infants exposed to high morphine levels from breast milk have died from breathing problems, extreme sleepiness, and inability to feed. There have been at least 10 documented infant deaths linked to codeine in breast milk since 2012. Tramadol has caused similar cases. The FDA says these drugs are not recommended - not because they’re always dangerous, but because you can’t predict who’s at risk.
What About Other Opioids? Are They Safe?
If you need something stronger than ibuprofen or acetaminophen - say, after a C-section or severe tearing - not all opioids are off-limits. Morphine is the safest opioid option for breastfeeding. It’s poorly absorbed by babies’ guts: only 0.5-1% of what’s in your milk actually gets into their bloodstream. That’s why it’s the go-to choice in hospitals for postpartum pain when opioids are needed.
Oxycodone is also used, but with caution. It transfers into milk at 0.1-0.5% of the maternal dose. The risk? Drowsiness in the baby. If your baby is unusually sleepy, struggles to latch, or feeds less than usual, stop and call your doctor.
Hydrocodone, hydromorphone, and fentanyl are considered "moderately safe" - but only for short-term use. Never use them longer than 4-6 days. And never combine them with other sedatives like alcohol or sleeping pills. Your baby’s brain is still developing. Even small amounts can slow breathing.
Timing Matters: When to Take Medication for Least Baby Exposure
It’s not just about which drug you take - it’s when you take it. If you’re using an opioid, timing your doses around feedings reduces your baby’s exposure.
Take your opioid dose right after you finish nursing. That gives your body time to break down the drug before the next feeding. Peak levels in breast milk happen 1-2 hours after you take the pill. So if you feed at 7 p.m., take your pain pill at 8 p.m. The next feeding is at 11 p.m. - by then, the drug concentration in your milk has dropped significantly.
For acetaminophen and ibuprofen, timing doesn’t matter as much. You can take them before, during, or after feeding. They’re so safe that you don’t need to wait. But if you’re on an opioid, treat it like a clock. Dose after feeding. Watch your baby. Wait.
What About Naproxen, Indomethacin, or Other NSAIDs?
Naproxen and indomethacin are NSAIDs, like ibuprofen - but they’re not recommended for breastfeeding mothers. Why? They stick around longer. Naproxen can build up in breast milk over time, reaching concentrations of 1.5-2.0% of the maternal dose after 24 hours. That’s higher than ibuprofen, and it’s risky for newborns, especially premature babies whose livers can’t clear drugs well.
Indomethacin is even trickier. It’s sometimes used to close a baby’s patent ductus arteriosus (a heart condition), but that’s only under strict medical supervision. It’s not meant for routine pain relief in nursing moms. Stick with ibuprofen. It’s shorter-acting, safer, and better studied.
What Signs Should You Watch For in Your Baby?
If you’re on any opioid - even morphine or oxycodone - watch your baby closely for the first 24 hours after each dose. Look for:
- Excessive sleepiness - so much that they won’t wake to feed
- Difficulty latching or sucking
- Slow or shallow breathing
- Unusual fussiness or limpness
- Constipation or reduced stooling
If you see any of these, stop the medication and call your doctor or pediatrician immediately. Don’t wait. Opioid overdose in infants can happen fast. And sometimes, the signs are subtle - a baby who just seems "too quiet."
Even if you’re only taking one dose, monitor your baby. Effects can be delayed. A single accidental dose of codeine might not cause harm - but it might. That’s why the advice is clear: avoid it entirely.

What About Pump and Dump?
You’ve probably heard this: "Pump and dump after anesthesia." That advice is outdated. The Academy of Breastfeeding Medicine updated its guidelines in 2021 to remove this recommendation entirely. Why? Because the amount of medication in breast milk after surgery is so tiny that it doesn’t affect the baby. Pumping and dumping doesn’t make it safer - it just makes you more tired and reduces your milk supply.
Same goes for acetaminophen, ibuprofen, and even morphine. You don’t need to discard milk. You can keep feeding. The only time you might consider pumping and dumping is if you accidentally took codeine or tramadol - and even then, it’s not always necessary. Talk to your doctor. They can help you decide based on the dose and timing.
What’s the Best Strategy for Postpartum Pain?
Here’s a simple, step-by-step plan that works:
- Start with ibuprofen and acetaminophen. Alternate every 3 hours. Use the lowest effective dose.
- If you need more, ask for morphine - not codeine or tramadol. Avoid oxycodone unless absolutely necessary.
- Take opioids right after feeding. Never before.
- Use opioids for no more than 4-6 days. Switch back to ibuprofen and acetaminophen as soon as you can.
- Watch your baby for drowsiness, breathing issues, or feeding problems.
- Don’t pump and dump unless your doctor tells you to.
Most women don’t need opioids at all. A combination of ibuprofen and acetaminophen is enough for 90% of postpartum pain - even after C-sections. The Michigan OPEN initiative found that replacing the first three doses of oral NSAIDs with IV Toradol (ketorolac) in the first 24 hours after surgery helped reduce opioid use by over 50%. That’s a powerful alternative.
What’s Next? Genetic Testing and Future Options
Right now, we can’t predict who will metabolize codeine dangerously. But research is changing that. Mayo Clinic published a 2023 study showing that a simple genetic test for CYP2D6 - the enzyme that processes codeine - could identify ultra-rapid metabolizers before prescribing. It’s not standard yet. But in the next few years, this could become routine.
For now, the best protection is knowledge. Know your options. Know the risks. Ask your doctor: "Is this safe for breastfeeding?" If they say "codeine" or "tramadol," push back. Say, "I’ve read the FDA warnings. Is there another option?"
You’re not being difficult. You’re being smart. And your baby deserves that.
Can I take ibuprofen while breastfeeding?
Yes. Ibuprofen is one of the safest pain medications for breastfeeding mothers. Only 0.6-0.7% of the dose passes into breast milk, and it doesn’t affect your baby’s sleep, feeding, or development. It’s recommended as a first-line choice by the American College of Obstetricians and Gynecologists and the Academy of Breastfeeding Medicine.
Is acetaminophen safe for breastfeeding moms?
Yes. Acetaminophen is considered very safe during breastfeeding. Only 0.1-1.0% of the maternal dose enters breast milk, and it clears quickly. It doesn’t reduce milk supply or cause drowsiness in infants. It’s often used alongside ibuprofen for better pain control.
Why is codeine dangerous while breastfeeding?
Codeine is converted into morphine in the body, but some women - about 1 in 100 - have a genetic variation that turns it into morphine too quickly. This can cause dangerously high levels of morphine in breast milk, leading to life-threatening breathing problems, extreme sleepiness, or even death in infants. The FDA warns that breastfeeding is not recommended while taking codeine.
Can I take tramadol while breastfeeding?
No. Tramadol is not recommended for breastfeeding mothers. It’s converted into an active metabolite (M1) that can build up in breast milk and cause severe respiratory depression in infants. The FDA has issued multiple safety warnings since 2018, citing cases of infant deaths linked to tramadol use during breastfeeding.
Should I pump and dump after taking pain meds?
No - not for ibuprofen, acetaminophen, or morphine. Pumping and dumping doesn’t make these drugs safer. It only reduces your milk supply and adds stress. The only exception is if you accidentally take codeine or tramadol - then contact your doctor. They may advise pumping and dumping temporarily, but it’s not always needed.
How long can I safely use opioids after birth?
Use opioids for no more than 4-6 days. After that, switch back to ibuprofen and acetaminophen. Long-term opioid use increases the risk of dependency and side effects in both you and your baby. If pain lasts longer than a week, talk to your doctor about other causes - it might not be normal postpartum pain.
What if my baby is premature or under 2 months old?
Premature babies and infants under 2 months have underdeveloped livers and kidneys, so they clear drugs much slower. Avoid all opioids if possible. If you must use them, use the lowest dose for the shortest time. Morphine is still the safest option, but monitor your baby even more closely. Always consult your pediatrician before giving any medication to a newborn.






Angel Tiestos lopez
January 15, 2026bro i just took ibuprofen after my c-section and my baby slept for 5 hours straight 😅 i thought i killed him lmao. turns out he was just chill. peace out, moms. you got this. 🙌