When you see an expiration date on a pill bottle, you assume that after that date, the medicine stops working. But what if that date is just a guess? The Military Shelf Life Extension Program (SLEP) proves that many drugs remain effective for years - sometimes over a decade - past their labeled expiration dates. This isn’t science fiction. It’s real data from government labs that have tested thousands of medications under strict conditions. And the results are changing how we think about drug storage, waste, and readiness.
Why Does the Military Care About Expired Drugs?
The U.S. Department of Defense keeps massive stockpiles of medicines for emergencies: chemical attacks, pandemics, battlefield injuries. These aren’t just backup supplies - they’re lifelines. But drugs cost money. Replacing them every two or three years, as manufacturers recommend, adds up fast. Between 2005 and 2015, the federal government spent billions replacing perfectly good drugs just because their labels said so. That’s where SLEP came in. Started in 1986, SLEP was created after early tests showed that drugs stored properly didn’t break down as quickly as expected. Instead of throwing them out, the military began testing them. The goal? Prove they still work. And they did - often by a wide margin.How SLEP Works: Science Over Guesswork
SLEP doesn’t rely on manufacturer labels. It uses real science. Here’s how it works:- Federal agencies nominate drugs from stockpiles for testing - things like antibiotics, antivirals, epinephrine, and painkillers.
- The FDA collects samples from sealed, properly stored containers.
- These samples are tested in controlled labs for potency, purity, and chemical breakdown.
- To qualify for extension, a drug must retain at least 85% of its original strength.
- If it passes, the FDA approves a new expiration date - often extending it by 2 to 5 years.
This isn’t a one-time check. Testing happens every 1 to 3 years. The program tracks each lot number, storage condition, and packaging type. That’s key: extension only applies to the exact same drug, in the same container, stored the same way. You can’t take a pill from your medicine cabinet and assume it’s good because SLEP says so.
The Numbers Don’t Lie
The data from SLEP is staggering:- Between 2005 and 2015, SLEP saved the federal government an estimated $2.1 billion by avoiding unnecessary replacements.
- A 2006 study in the Journal of Pharmaceutical Sciences found 88% of 122 tested drugs were still stable beyond their expiration dates - some for over 15 years.
- By 2022, over 2,500 different drug products had received shelf-life extensions.
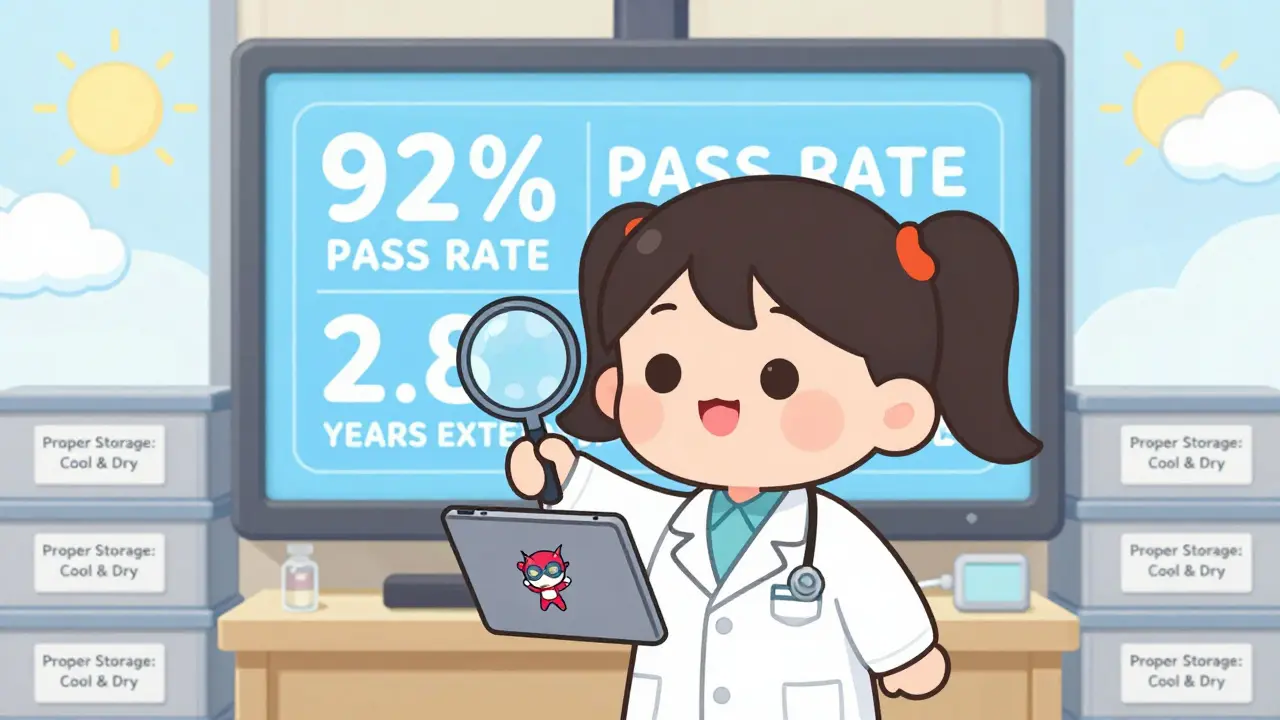
- 92% of tested lots in 2021 qualified for extension, averaging 2.8 years added per cycle.
Compare that to the commercial world. In 2019, a study in Health Affairs estimated that expired drugs thrown away in U.S. hospitals and pharmacies cost $1.7 billion annually. The military’s approach doesn’t just save money - it saves lives by ensuring critical medicines are available when needed.
What Drugs Last? What Doesn’t?
Not all drugs behave the same. SLEP has found that some are incredibly stable:- Antibiotics like doxycycline and ciprofloxacin often retain full potency for over a decade.
- Antivirals such as oseltamivir (Tamiflu) have been extended by 3 years in multiple cycles.
- Epinephrine auto-injectors (EpiPens) were tested and found to retain over 90% potency 10+ years past expiration.
- Analgesics like acetaminophen and ibuprofen show almost no degradation under proper storage.
On the flip side, some drugs are more fragile:
- Insulin and other biologics degrade faster - though since 2021, SLEP has started testing select biologics under strict conditions.
- Liquid formulations, especially those requiring refrigeration, are less stable than solid tablets.
- Drugs in non-sealed containers or exposed to heat, moisture, or light rarely qualify.
Storage matters more than the expiration date. A drug stored in a cool, dry, dark place - like a military depot - lasts far longer than one left on a bathroom counter.
Why Can’t You Use SLEP to Extend Your Medicine?
You might be thinking: “If the military can do it, why can’t I?”Because SLEP isn’t a consumer program. It’s a tightly controlled government operation with three non-negotiable rules:
- Testing only happens on sealed, original packaging from verified stockpiles.
- Each extension applies to one specific lot number - not all versions of the drug.
- Storage conditions must match the exact environment used in testing (typically 20-25°C, low humidity, no light exposure).
The FDA explicitly warns against generalizing SLEP results to personal use. A pill from your pharmacy might look identical, but if it was stored in a hot car or a humid drawer, it could be degraded. SLEP doesn’t certify your medicine - it certifies government stockpiles.
The Bigger Picture: Global Impact
SLEP didn’t just save money - it changed global standards. Since 2010, 12 NATO countries have built their own shelf-life extension programs using SLEP’s model. Australia, Canada, and the UK now test their own stockpiles with similar protocols. Even the World Health Organization has referenced SLEP data in its guidelines for emergency medical supplies.It’s also pushing the pharmaceutical industry to rethink expiration dates. Dr. Lawrence Yu, former FDA deputy director, said SLEP data “fundamentally changed our understanding of drug stability.” That’s why the FDA now uses SLEP findings to inform its own research - not to change consumer labels, but to improve how drugs are tested and stored long-term.

Challenges and Criticisms
SLEP isn’t perfect. Some experts warn against overgeneralizing its results. Dr. Michael D. Swartzburg from UCSF points out: “The program tests ideal conditions. Real-world storage? Not so much.”There are also logistical hurdles. A 2018 survey of military logistics staff found that 35% had trouble accessing the SLEP database because of outdated access systems. It took over 7 days on average to get the data they needed. In 2022, the DoD and FDA rolled out a new electronic system that cut approval time from 14 months to 8 - a major improvement.
Another issue? Funding. The 2023 National Defense Authorization Act wants to expand SLEP to cover more chemical and biological countermeasures. But that could cost $75 million more per year. With new threats emerging, the program needs to evolve - faster.
What’s Next for Drug Stability?
The FDA’s 2022-2026 plan includes using advanced tools like mass spectrometry and accelerated stability testing to predict how drugs degrade. The goal? Move from reactive testing to predictive modeling. Instead of waiting for a drug to expire, scientists want to forecast its lifespan based on chemistry, packaging, and storage history.This could one day lead to smarter expiration dates - not just for the military, but for everyone. Imagine a pill bottle with a QR code that tells you its real stability status based on how it was stored. That’s not fantasy anymore. SLEP is laying the groundwork.
Final Takeaway
The Military Shelf Life Extension Program shows us something powerful: expiration dates aren’t magic cutoffs. They’re conservative estimates based on limited testing. Real-world stability? Often much longer - if you store the drug right.For the military, SLEP is a smart, science-backed way to keep life-saving drugs ready without wasting billions. For the rest of us? It’s a reminder to think critically about what we’re told. A date on a bottle doesn’t tell the whole story. Storage, chemistry, and evidence matter more.
Do all drugs last beyond their expiration dates?
No. While many solid medications like antibiotics, painkillers, and antivirals remain stable for years, others - especially biologics like insulin, liquid suspensions, or refrigerated products - degrade faster. SLEP only extends shelf life for drugs that pass strict testing under controlled conditions. You can’t assume any expired drug is still safe or effective.
Can I use SLEP data to extend the life of my home medicine?
No. SLEP extensions apply only to specific lots tested under government-controlled storage conditions. Your medicine was likely stored differently - in a bathroom, car, or kitchen - which can accelerate degradation. The FDA warns against using SLEP results to justify taking expired personal medications. The risks outweigh any potential benefit.
How often are drugs tested under SLEP?
Testing typically occurs every 1 to 3 years, depending on the drug’s stability history. Drugs with a track record of long-term stability may be tested less frequently. The average testing cycle time is now about 11.4 months, thanks to improved systems introduced in 2022.
What percentage of drugs qualify for extension?
In 2021, 92% of tested lots qualified for shelf-life extension. This high success rate reflects the effectiveness of proper storage and the inherent stability of many pharmaceutical compounds. However, failure rates rise sharply if storage conditions deviate from standards.
Has SLEP influenced commercial drug expiration dates?
Not directly. Manufacturers still use conservative 2-3 year labels for legal and liability reasons. But SLEP data has influenced how the FDA designs its own stability studies and how emergency stockpiles are managed worldwide. It’s slowly changing the science behind expiration dating - even if consumer labels haven’t caught up yet.
For now, the best advice remains: store your medicines properly - cool, dry, and out of sunlight. And if you’re unsure about an expired drug, don’t guess. Talk to a pharmacist. Your health isn’t worth the risk.