Every year, millions of people in the UK and beyond take over-the-counter (OTC) medicines without thinking twice. A headache? Grab an ibuprofen. Stuffy nose? Reach for a cold tablet. Trouble sleeping? Diphenhydramine is on the shelf. But here’s the problem: OTC medications aren’t harmless. When mixed with your prescription drugs, they can turn a simple remedy into a medical emergency.
You might not realize it, but 67% of patients never tell their doctor what OTC meds they’re taking. That’s not just a gap in communication-it’s a silent risk. The result? Unintentional overdoses, dangerous drops in blood pressure, liver failure, internal bleeding, and even strokes. And it’s not rare. Drug interactions are behind nearly 7% of all hospital admissions in the UK and US.
What Exactly Is an OTC-Prescription Drug Interaction?
An interaction happens when one substance changes how another works in your body. With OTC meds and prescriptions, this can mean:
- Your blood thinner stops working because you took ibuprofen
- Your antidepressant causes serotonin overload after you used a common cough syrup
- Your stomach ulcer worsens because you combined aspirin with a prescription steroid
- Your blood pressure spikes after eating aged cheese while on an MAO inhibitor
These aren’t theoretical risks. They’re real, documented, and often preventable.
The Three Most Dangerous OTC Medication Classes
1. NSAIDs: Ibuprofen, Naproxen, Aspirin
These are the most common OTC painkillers-and the most dangerous when mixed with prescriptions.
- With blood thinners (warfarin, apixaban): Bleeding risk increases 2 to 4 times. Even a small cut can lead to serious blood loss.
- With high blood pressure meds (lisinopril, losartan): NSAIDs can make your BP rise by 5-15 mmHg, undoing months of treatment.
- With low-dose aspirin (for heart protection): Taking ibuprofen or naproxen right after aspirin blocks aspirin’s ability to protect your heart. If you take aspirin daily for heart health, take it at least 30 minutes before any other NSAID-or avoid NSAIDs entirely.
- With antidepressants (SSRIs like sertraline): This combo increases stomach bleeding risk by 3 to 10 times. It’s one of the most overlooked dangers.
And here’s the kicker: many people don’t know they’re taking NSAIDs. Cold and flu tablets, period pain remedies, and even some arthritis gels contain ibuprofen or naproxen. Always check the active ingredients.
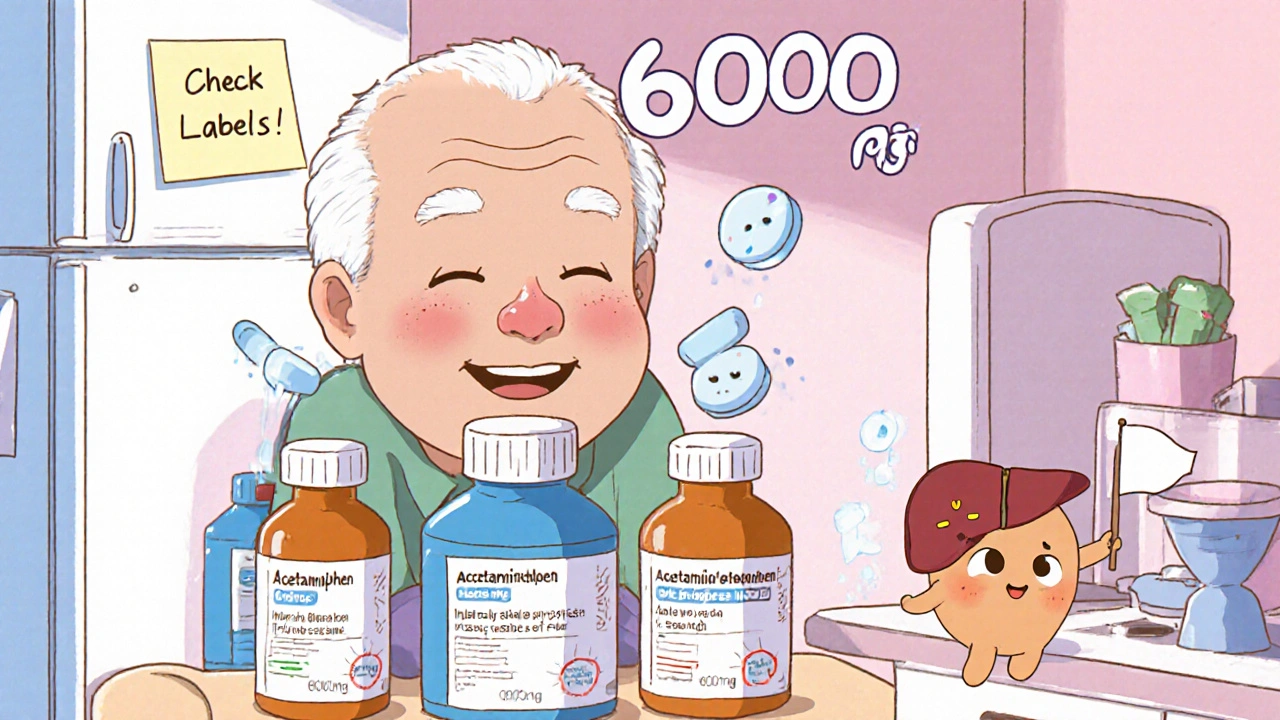
2. Acetaminophen (Paracetamol)
Acetaminophen is safe-if you don’t overdose. The problem? It’s in over 200 different products: cold remedies, sleep aids, migraine pills, and even some prescription painkillers like co-codamol.
The maximum safe daily dose is 4,000 mg. But people routinely hit 6,000-8,000 mg without realizing it. One woman in Bristol took three different cold medicines over three days. Each had 500 mg of acetaminophen. She ended up in the hospital with acute liver failure. She didn’t have a history of alcohol use or liver disease. Just too many pills.
Here’s how to avoid it:
- Never take two products with acetaminophen at the same time
- Check every label-even if it’s "natural" or "herbal"
- If you’re on prescription painkillers, ask if they already contain acetaminophen
3. Antihistamines: Diphenhydramine, Chlorpheniramine
First-generation antihistamines like diphenhydramine (Benadryl) are in sleep aids, allergy pills, and motion sickness tablets. They cause drowsiness, dry mouth, and blurred vision. That’s bad enough alone. But combine them with:
- Prescription sedatives (diazepam, zopiclone)
- Antidepressants (trazodone, mirtazapine)
- opioid painkillers (codeine, oxycodone)
And you’re looking at extreme drowsiness, slowed breathing, falls, and even coma. Elderly patients are especially at risk. One study found that 1 in 5 hospital admissions for falls in people over 65 were linked to OTC sleep aids mixed with prescription meds.
Other Dangerous Combinations You Might Not Know About
- Levothyroxine (thyroid meds) + omeprazole (acid reducer): Omeprazole can block thyroid hormone absorption. You might think your dose is wrong-but it’s the antacid.
- Clopidogrel (blood thinner) + omeprazole: Omeprazole reduces clopidogrel’s effectiveness by up to 50%. If you’ve had a stent or heart attack, this combo could mean another clot.
- Diuretics (furosemide) + sodium phosphate laxatives: This mix can cause acute kidney injury, especially in older adults or those with existing kidney problems.
- MAO inhibitors (antidepressants like phenelzine) + aged cheese, cured meats, red wine: This isn’t even a drug-drug interaction-it’s food-drug. It can cause a sudden, deadly spike in blood pressure.
- Statins (atorvastatin) + grapefruit juice: Grapefruit blocks the enzyme that breaks down statins. This can lead to muscle damage and kidney failure.
Who’s at Highest Risk?
Not everyone is equally vulnerable. These groups need to be extra careful:
- People over 65: On average, they take 5+ medications daily. More drugs = more chances for conflict.
- People with kidney or liver disease: These organs clear drugs from your body. If they’re not working well, drugs build up dangerously.
- People with heart disease, diabetes, or high blood pressure: These conditions often require multiple medications. One wrong OTC pick can undo your control.
- People taking antidepressants or anticoagulants: These drugs have narrow safety margins. Small changes can have big effects.
What You Should Do Right Now
Don’t wait for a problem to happen. Here’s your action plan:
- Make a full list: Write down every prescription, OTC, vitamin, herb, and supplement you take. Include the dose and why you take it.
- Take it to your pharmacist: Pharmacists are trained to spot interactions. They see hundreds of these cases every week. Ask them to check your list. Do this every time you start a new medicine.
- Read every label: Look for the "active ingredients" section. If two products have the same one, don’t take them together.
- Use the NHS Medicines Checker: The NHS website has a free tool that checks interactions between your meds. It includes OTCs and supplements.
- Ask two questions before taking anything new: "Does this interact with any of my prescriptions?" and "Is there another option that won’t interfere?"
Why Pharmacists Are Your Best Defense
Doctors are busy. They might not know you’re taking a daily antihistamine for allergies or a weekly laxative. Pharmacists? They see your full medication history. They’re the ones who catch the overlap between your cold medicine and your blood pressure pill.
In the UK, you can walk into any pharmacy and ask for a free Medicines Use Review (MUR). It’s a 10-15 minute chat where they go through your meds, spot risks, and give you a written summary. No appointment needed. And if you’re on multiple prescriptions, you’re entitled to this service every year.
What’s Changing? What You Should Watch For
The FDA and UK’s MHRA have started pushing for clearer OTC labels. New packaging now includes warnings like:
- "May increase bleeding risk if taken with warfarin"
- "Do not take with other products containing acetaminophen"
- "May reduce effectiveness of thyroid medication"
But not all products have updated labels yet. And many people still ignore them. That’s why you can’t rely on packaging alone.
Future tools are coming-apps that scan your pill bottles and flag risks, electronic health records that include OTC use. But for now, the best tool is still you: informed, alert, and asking questions.
Final Thought: OTC Doesn’t Mean Risk-Free
Just because you don’t need a prescription doesn’t mean it’s safe. Your body doesn’t care if a drug is sold over the counter or behind the pharmacy counter. It reacts the same way.
If you’re taking any prescription meds-especially for heart, blood pressure, depression, or blood thinning-assume every OTC medicine could interact. Always check. Always ask. Your life might depend on it.
Can I take ibuprofen with my blood thinner?
No, not without medical supervision. Ibuprofen and other NSAIDs significantly increase the risk of serious bleeding when taken with blood thinners like warfarin, apixaban, or rivaroxaban. Even occasional use can be dangerous. If you need pain relief, ask your doctor about paracetamol (acetaminophen) instead-but even that has limits if you’re on multiple meds.
Is it safe to take cold medicine if I’m on antidepressants?
It depends. Many cold medicines contain dextromethorphan, pseudoephedrine, or diphenhydramine-all of which can interact dangerously with antidepressants. Dextromethorphan combined with SSRIs or SNRIs can cause serotonin syndrome-a life-threatening condition with symptoms like confusion, rapid heart rate, and high fever. Always check the active ingredients and consult your pharmacist before taking any cold remedy.
Why can’t I take antacids with my thyroid medication?
Antacids containing aluminum, magnesium, or calcium can bind to levothyroxine in your gut and stop it from being absorbed. This means your thyroid hormone levels drop, even if you’re taking your dose correctly. To avoid this, take your thyroid pill at least 4 hours before or after any antacid, calcium supplement, or iron tablet.
Can I use herbal supplements with my prescriptions?
Many herbal supplements interact with prescription drugs. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and blood thinners. Garlic and ginkgo can increase bleeding risk when taken with aspirin or warfarin. Even green tea can interfere with some heart medications. Always tell your pharmacist about every supplement you take-even if you think it’s "natural" and harmless.
How do I know if I’ve taken too much acetaminophen?
Symptoms of acetaminophen overdose don’t always show up right away. You might feel fine for 24-48 hours. Then nausea, vomiting, loss of appetite, and pain under your right ribs appear. By then, liver damage may already be serious. If you’ve taken more than 4,000 mg in 24 hours-or took multiple products containing acetaminophen-seek medical help immediately. Don’t wait for symptoms.
What should I do if I accidentally took a dangerous combination?
Call NHS 111 or your local pharmacy immediately. Don’t wait for symptoms. If you’re having trouble breathing, chest pain, confusion, or severe drowsiness, call 999. Even if you feel fine, the interaction could still be building inside your body. Early intervention can prevent serious harm.






steffi walsh
November 18, 2025Just wanted to say THANK YOU for this post-it’s the kind of thing I wish my grandma had read before she started mixing her blood pressure meds with that "natural" sleep aid. I’ve seen too many people assume "over-the-counter" means "harmless." You nailed it. 🙏