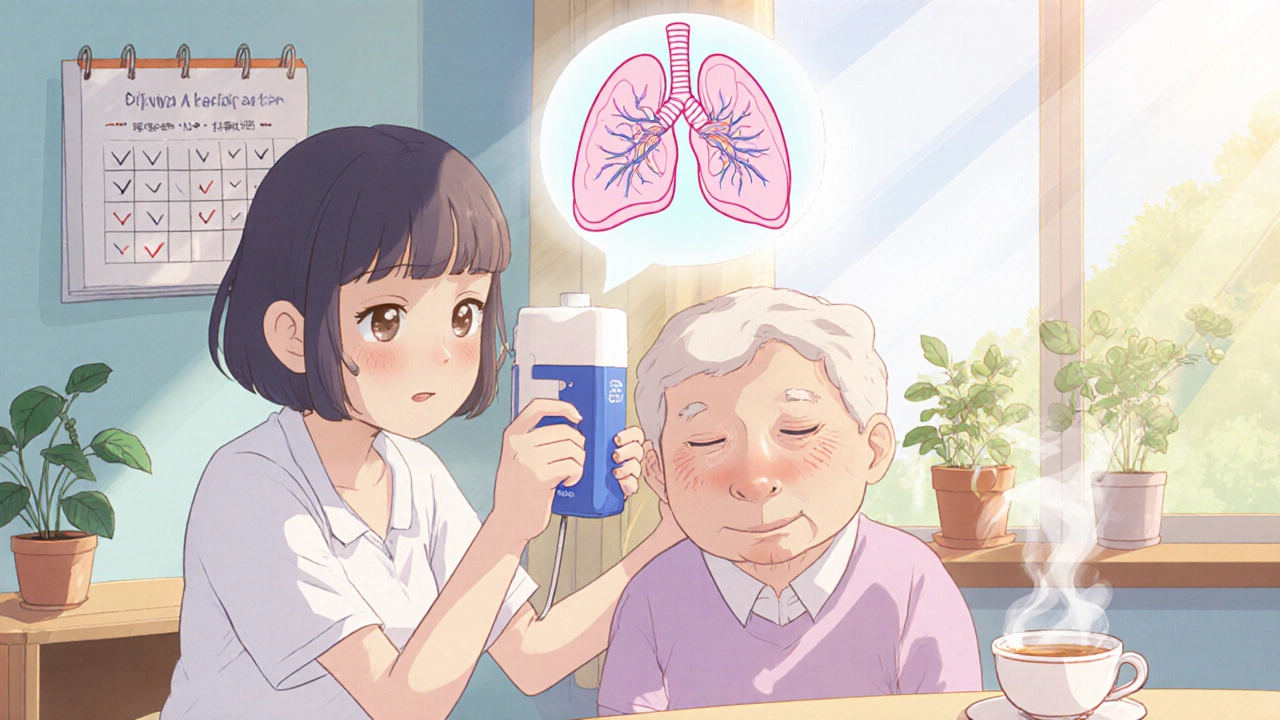
When someone you care for has COPD, every breath matters. Tiotropium bromide isn’t a cure, but for many, it’s the difference between struggling to get through the day and being able to sit outside, take a walk, or even sleep without waking up gasping. If you’re helping a loved one manage this condition, understanding how tiotropium bromide works-and how to use it right-isn’t just helpful. It’s essential.
What Is Tiotropium Bromide?
Tiotropium bromide is a long-acting bronchodilator used to treat chronic obstructive pulmonary disease, or COPD. It’s not for sudden attacks. You won’t use it when someone’s wheezing and panicking. Instead, it’s taken once a day to keep airways open over time. Think of it like a daily lock on a door that keeps it from slamming shut.
This medication works by blocking muscarinic receptors in the lungs. That sounds technical, but here’s what it means in plain terms: it stops the muscles around the airways from tightening up. When those muscles relax, air flows more freely. People using tiotropium bromide often report less shortness of breath, fewer flare-ups, and better sleep.
It comes in two main forms: the Spiriva Handihaler and the Spiriva Respimat. Both deliver the same drug, but in very different ways. One uses a dry powder you inhale from a capsule. The other uses a fine mist you spray into your mouth. Which one your loved one uses depends on their doctor’s choice and how well they can handle the device.
How to Use the Handihaler Correctly
If your loved one uses the Handihaler, you’ll see a small plastic device with a mouthpiece and a capsule chamber. It looks simple, but mistakes here can mean the medicine doesn’t reach the lungs.
- Open the device by sliding the thumb grip away from you.
- Take one capsule out of its foil pack just before use. Never store capsules outside the foil-they lose strength fast.
- Place the capsule in the chamber. Don’t swallow it. Don’t pierce it yet.
- Close the device until you hear a click. This primes the piercing mechanism.
- Hold the device upright and breathe out fully-away from the mouthpiece.
- Put the mouthpiece in their mouth and close lips tightly. Press the green button once. This pierces the capsule.
- Inhale slowly and deeply through the mouth. Don’t breathe through the nose.
- Hold breath for 5 to 10 seconds, then breathe out slowly.
- Open the device, check if the capsule is empty. If powder remains, repeat steps 5-8.
- Throw the used capsule away. Wash the mouthpiece weekly with a dry cloth.
Most people get it wrong on step 7. They breathe too fast or too shallow. The powder needs a slow, deep inhale to reach deep into the lungs. If they cough right after, it’s likely they didn’t inhale properly.
How to Use the Respimat Correctly
The Respimat is a small, metal inhaler that looks like a pen. It sprays a mist instead of powder. Many older adults prefer this because it’s easier to coordinate.
- Remove the clear base and insert the cartridge.
- Turn the base clockwise until it clicks (full turn). Do this twice to prime the device.
- Hold the inhaler upright. Point the mouthpiece away from you.
- Press the gray button once to release a spray. You should hear a click and see a mist.
- Breathe out fully, then place lips tightly around the mouthpiece.
- Inhale slowly and deeply as you press the button again.
- Hold breath for 5-10 seconds. Breathe out slowly.
- Replace the cap. Clean the mouthpiece weekly with a dry tissue.
Don’t shake it. Don’t spray it into the air to test it. Each spray is a full dose. If they spray twice by accident, they’ve wasted half the day’s medication.
When to Take It-and When Not To
Tiotropium bromide is taken once a day, at the same time every day. Morning is best for most people-it helps them breathe easier through the day. But consistency matters more than timing.
Never use it for sudden breathing trouble. If your loved one has a flare-up, they need a rescue inhaler like salbutamol. Tiotropium doesn’t work fast enough. If they’re using their rescue inhaler more than twice a week, talk to the doctor. Their COPD may be getting worse.
Also, don’t stop it just because they feel better. COPD doesn’t go away. Skipping doses lets airways tighten again. It’s not like a painkiller you take when it hurts. This is maintenance.

Side Effects to Watch For
Most people tolerate tiotropium well. But some side effects happen. You don’t need to panic over every little thing-but you do need to know when to call the doctor.
- Very common: Dry mouth. This is normal. Keep water nearby. Sugar-free gum helps.
- Common: Sore throat, hoarse voice. Rinse mouth with water after each use.
- Less common: Blurred vision, trouble urinating. This is more likely in older men with prostate issues.
- Rare but serious: Sudden wheezing after use. If this happens, stop the inhaler and call emergency services. It could be a paradoxical reaction.
If your loved one has glaucoma or an enlarged prostate, tell their doctor before starting. Tiotropium can make these worse. It’s not a deal-breaker-but they need to be monitored.
What to Do If They Miss a Dose
Missed one day? Don’t double up. Just give the next dose at the regular time. Doubling up doesn’t help. It just raises the risk of side effects.
If they miss more than two days in a row, call the doctor. They may need a quick check-up to make sure their lungs haven’t tightened up too much.
Storage and Safety Tips
Keep both devices at room temperature. Don’t freeze them. Don’t leave them in a hot car. Heat and moisture ruin the medicine.
Store capsules in the original foil pack until use. Exposure to air cuts their effectiveness.
Keep inhalers out of reach of children. Even a single dose can be dangerous for a toddler.
Check expiration dates. The Respimat device lasts 3 months after first use. The Handihaler lasts until the capsules expire. Never use expired capsules.

When to Call the Doctor
You don’t need to call for every small change. But here are signs you shouldn’t ignore:
- More frequent use of rescue inhaler (more than 2-3 times a week)
- New or worsening wheezing after using tiotropium
- Difficulty urinating or painful urination
- Eye pain, redness, or blurred vision
- Swelling of the face, lips, or tongue
If any of these happen, don’t wait. Call the GP or go to urgent care. Early action prevents hospital visits.
Helping Them Stick With It
The biggest problem with tiotropium isn’t the medicine. It’s the habit. People forget. They get discouraged. They think, “I feel fine, why keep taking this?”
Here’s what helps:
- Set a daily alarm on their phone or use a pill organizer with a morning slot.
- Keep the inhaler next to their toothbrush or coffee maker-something they do every day.
- Track usage. Some devices have counters. If not, mark a calendar.
- Ask them how they feel after a week. Often, they don’t notice improvement until they stop and then restart.
Don’t nag. Be a partner. Say, “Let’s check your inhaler today,” instead of, “You forgot again.”
Other Treatments That Work With It
Tiotropium is rarely used alone. Most people also use:
- A short-acting rescue inhaler (like salbutamol) for sudden symptoms
- Inhaled steroids (like fluticasone) if they have frequent flare-ups
- Combination inhalers that include tiotropium plus another long-acting drug
Some newer options like umeclidinium or vilanterol are similar but not interchangeable. Never switch without talking to the doctor.
Also, pulmonary rehab-breathing exercises, light exercise, nutrition advice-is just as important as the inhaler. Ask if your loved one can join a program. Many are free through the NHS.
Final Thought: It’s Not Just About the Inhaler
Tiotropium bromide is a tool. It helps, but it doesn’t fix everything. Smoking cessation is still the most powerful thing you can do for COPD. If your loved one smokes, help them quit. Even if they’ve smoked for 40 years, quitting now still adds years to their life.
Also, watch for infections. A cold or flu can turn into a hospital trip for someone with COPD. Get flu shots every year. Ask about the pneumococcal vaccine too.
And remember: your calm matters. When someone is struggling to breathe, panic spreads fast. Your steady voice, your patience, your willingness to learn-those are the things that make the biggest difference.
Can tiotropium bromide be used for asthma?
No. Tiotropium bromide is approved only for COPD, not asthma. While it may help some asthma patients off-label, it’s not the standard treatment and can mask worsening symptoms. Always follow the doctor’s prescribed plan.
How long does it take for tiotropium to start working?
It doesn’t work right away. Most people notice less shortness of breath after 1 to 2 weeks. Full benefits take 4 to 6 weeks. It’s not meant for quick relief, so don’t expect instant results.
Can I use tiotropium with a spacer?
No. Spacers are designed for metered-dose inhalers that spray mist, like salbutamol. The Handihaler uses dry powder, and the Respimat is already designed to deliver fine mist without a spacer. Using one with tiotropium will reduce the dose and make it less effective.
Is tiotropium bromide safe for elderly patients?
Yes, it’s commonly used in older adults. But they’re more likely to experience side effects like dry mouth, constipation, or trouble urinating. Monitor closely. Dose adjustments aren’t usually needed, but kidney or liver problems may require extra care.
What happens if I accidentally swallow the capsule?
If the capsule is swallowed whole, it won’t work. The medicine is designed to be inhaled, not digested. It won’t cause harm, but the dose is wasted. Use a new capsule and continue the next day as normal.




jerry woo
October 28, 2025Let me tell you something nobody else will: Big Pharma doesn't want you to know tiotropium's real cost. The Handihaler? Designed to make you buy new devices every three months. The Respimat? Same thing. They're milking the COPD crowd while you're too busy trying not to suffocate to notice. And don't get me started on the 'weekly cleaning' - that's just a loophole so they can sell you replacement mouthpieces. This isn't medicine, it's a subscription model with side effects.