Aspirin Isn’t for Everyone Anymore - Here’s Who Still Needs It
If you’re over 50 and have never had a heart attack or stroke, there’s a good chance you’ve been told to take a daily low-dose aspirin to protect your heart. Maybe your parents did it. Maybe your doctor suggested it years ago. But as of 2025, that advice has changed - dramatically.
For decades, aspirin was seen as a simple, cheap shield against heart disease. But new evidence shows that for most healthy people, the risks of bleeding outweigh the benefits. The aspirin therapy that once seemed like a no-brainer is now a carefully weighed decision - one that depends on your age, your risk factors, and your personal history.
What Aspirin Actually Does (And Doesn’t Do)
Aspirin works by stopping blood platelets from clumping together. That’s useful when you already have narrowed arteries - because clots can trigger heart attacks or strokes. But in people with healthy arteries, those same anti-clotting effects can cause dangerous bleeding.
Studies involving more than 130,000 people show aspirin reduces the chance of a nonfatal heart attack by about 12% and a nonfatal stroke by about 12%. But it also increases the risk of major bleeding - like bleeding in the stomach, brain, or intestines - by 43%. That’s not a small trade-off. For every 100 people taking aspirin daily for 10 years, roughly one might avoid a heart attack, but two might have a serious bleeding event that needs hospitalization or a blood transfusion.
The biggest shift came in 2022, when the U.S. Preventive Services Task Force (USPSTF) updated its guidelines. They now say: don’t start aspirin for heart disease prevention if you’re 60 or older. For people aged 40 to 59, it’s only worth considering if you have a high risk of heart disease and a low risk of bleeding - and even then, it’s not automatic.
Who Should Still Consider Aspirin?
Not everyone should stop. There are specific groups where the math still works.
- People aged 40-59 with a 10% or higher 10-year heart disease risk: This is calculated using your age, sex, race, blood pressure, cholesterol, whether you have diabetes, and if you smoke. If your risk hits or exceeds 10%, and you don’t have a history of ulcers, bleeding disorders, or are not on blood thinners, aspirin might help. But it’s not a guarantee - it’s a conversation.
- People with type 2 diabetes and additional risk factors: The American Diabetes Association still recommends aspirin for adults over 40 with diabetes who also have high blood pressure, high cholesterol, or smoke. Their risk of heart disease is so high that the potential benefit still tips the scale.
- People with familial hypercholesterolemia: This inherited condition causes extremely high cholesterol from birth. Even if they’re young, their artery damage starts early. Many lipid specialists recommend aspirin here, even under age 40.
For everyone else - especially those over 60 - the guidelines are clear: don’t start. If you’re already taking it, talk to your doctor before stopping.
Who Should Avoid Aspirin Completely?
Some people face such high bleeding risks that aspirin is dangerous, even if they have heart disease risk factors.
- Anyone with a history of stomach ulcers or GI bleeding
- People taking other blood thinners like warfarin, apixaban, or rivaroxaban
- Those with uncontrolled high blood pressure (systolic over 160)
- People who drink three or more alcoholic drinks daily
- Anyone over 60 without known heart disease
- People with kidney or liver disease
Doctors use a tool called the HAS-BLED score to measure bleeding risk. If your score is 3 or higher, aspirin is generally not recommended - no matter how high your heart disease risk is.
Why Did the Guidelines Change?
It’s not that aspirin stopped working. It’s that everything else got better.
Thirty years ago, many people didn’t take statins. Blood pressure wasn’t well controlled. Diabetes management was poor. Smoking was common. In that environment, aspirin’s modest benefit made sense.
Today, statins lower heart attack risk by 25-37%. Blood pressure medications reduce stroke risk by 40%. Quitting smoking cuts heart disease risk by half in just five years. With these tools, aspirin’s small edge doesn’t justify the bleeding risk.
One cardiologist put it plainly: “We used to give aspirin because we had nothing else. Now we have better tools - and aspirin’s side effects are no longer acceptable.”
What About Family History?
This is the most common reason people keep taking aspirin: “My dad had a heart attack at 55.”
Family history matters - but it’s not a magic pass. If your father had a heart attack at 55, you might have higher cholesterol, higher blood pressure, or insulin resistance. Those are the real risks. And those are what you need to treat - with statins, diet, exercise, and blood pressure control - not aspirin.
Aspirin doesn’t fix genetics. It just thins your blood. If your arteries are clean, thinning your blood won’t stop plaque from forming. If your arteries are already damaged, you’re probably already on a statin - and you don’t need aspirin unless you’ve had a prior event.
What Dose Should You Take?
If your doctor says aspirin is right for you, the dose is almost always 75-100 mg per day. That’s one “baby aspirin.” Higher doses - like 325 mg - don’t offer more protection but increase bleeding risk.
Don’t take enteric-coated aspirin thinking it’s safer for your stomach. Studies show it doesn’t reduce bleeding risk. The coating just delays absorption - it doesn’t protect your gut lining.
What If You’re Already Taking It?
If you’re over 60 and taking aspirin daily for prevention - with no history of heart attack, stroke, stent, or bypass - you should talk to your doctor about stopping.
Don’t quit cold turkey. Stopping suddenly can cause a rebound effect where platelets become hyperactive, slightly increasing short-term risk. Your doctor may recommend tapering off slowly, especially if you’ve been on it for years.
If you’re under 60 and have no bleeding risks, you might continue - but only if your 10-year heart disease risk is above 10%. If your risk is lower, stop. The benefit is too small to justify the danger.
What Are the Real Alternatives?
Aspirin isn’t the only tool - and it’s rarely the best one for prevention.
- Statins: The #1 drug for heart disease prevention. They lower LDL cholesterol, stabilize plaque, and reduce inflammation. Atorvastatin and rosuvastatin are the most prescribed.
- Blood pressure control: Keeping systolic pressure below 130 mmHg cuts stroke risk by 40%.
- Exercise: Just 150 minutes a week of brisk walking reduces heart disease risk by 30%.
- Healthy diet: Diets rich in vegetables, nuts, whole grains, and fish (like the Mediterranean diet) cut heart attack risk by up to 30%.
- Quitting smoking: Within one year, your heart attack risk drops by half.
These aren’t “alternatives” - they’re the foundation. Aspirin was never meant to replace them. It was meant to be a backup. And now, even that backup is reserved for very few.
What’s Next for Aspirin?
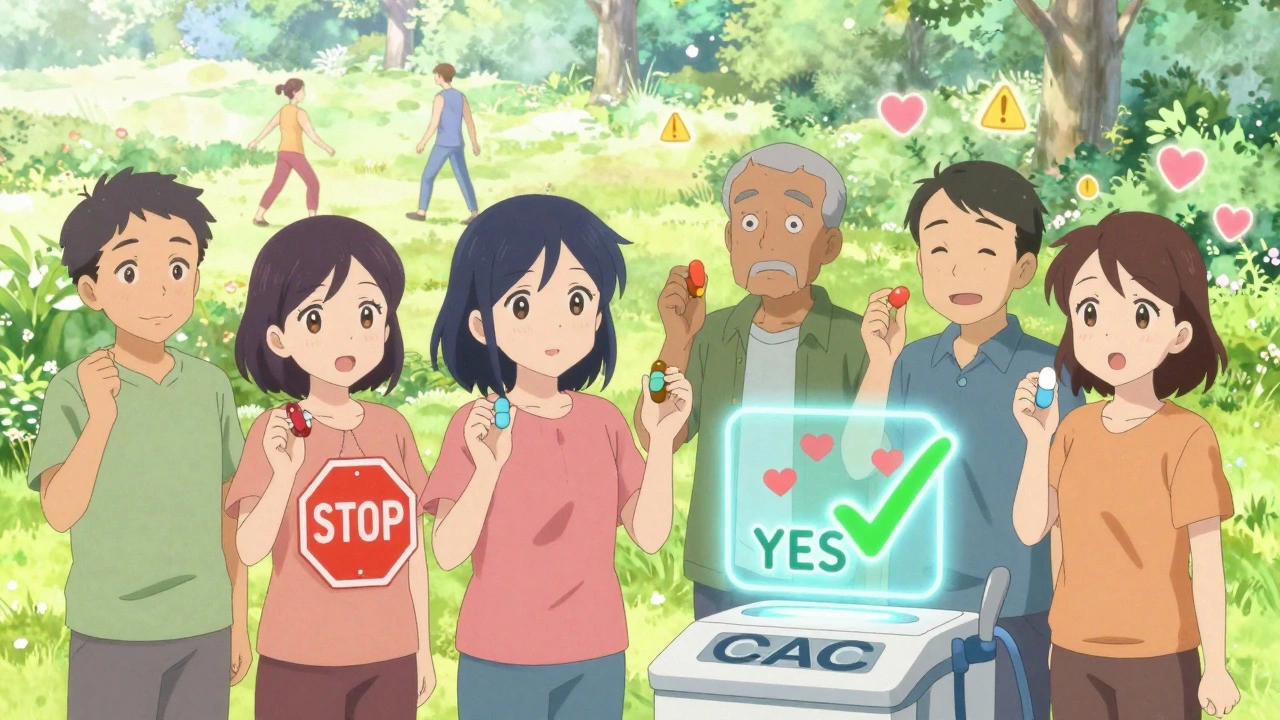
The American Heart Association is updating its guidelines in 2024. One big change? They may start using coronary artery calcium (CAC) scans to better identify who truly needs aspirin.
A CAC scan is a simple CT scan that shows calcium buildup in heart arteries. A score of zero means almost no plaque - and aspirin is pointless. A score over 100 means significant buildup - and aspirin might help. This could finally make aspirin use truly personalized.
For now, the message is simple: Aspirin for prevention is no longer a default. It’s a rare exception.
Frequently Asked Questions
Is it safe to take aspirin every day if I have no heart problems?
For most people without heart disease, no. Daily aspirin increases the risk of serious bleeding - especially in the stomach and brain - without offering enough protection. If you’re over 60, current guidelines say not to start. If you’re under 60, only consider it if your 10-year heart disease risk is 10% or higher and you have no bleeding risk factors.
I’ve been taking aspirin for 10 years. Should I stop?
If you’re over 60 and have never had a heart attack, stroke, or stent, yes - talk to your doctor about stopping. If you’re under 60 and have a high heart disease risk (10% or more) and no bleeding history, you may continue. But don’t stop suddenly. Work with your doctor to taper off safely if needed.
Does aspirin help prevent colon cancer?
Some studies suggest long-term aspirin use may lower colon cancer risk, but this is not a reason to start it. The bleeding risks still outweigh this potential benefit for most people. If you’re concerned about colon cancer, focus on screening - colonoscopies are proven, safe, and far more effective.
Can I take aspirin with other medications like ibuprofen?
Avoid taking ibuprofen or naproxen regularly if you’re on aspirin. These drugs can block aspirin’s antiplatelet effect. If you need pain relief, use acetaminophen (paracetamol) instead. If you must take ibuprofen, take it at least 30 minutes after your aspirin - or 8 hours before.
Is enteric-coated aspirin safer for my stomach?
No. Studies show enteric-coated aspirin doesn’t reduce the risk of stomach bleeding compared to regular aspirin. The coating delays absorption but doesn’t protect your stomach lining. Stick to low-dose (75-100 mg) and avoid higher doses entirely.
What to Do Next
If you’re unsure whether aspirin is right for you:
- Ask your doctor for your 10-year cardiovascular risk score using the ACC/AHA calculator.
- Review your bleeding risk - have you ever had a stomach ulcer? Are you on other blood thinners? Do you drink alcohol regularly?
- Discuss your family history - but don’t let it override your personal risk profile.
- Ask if a coronary artery calcium scan would help clarify your risk.
- Focus on proven prevention: statins if needed, blood pressure control, exercise, and quitting smoking.
Aspirin isn’t evil. It saves lives - but only in the right people. For most healthy adults today, it’s not a shield. It’s a liability. The best way to protect your heart isn’t a pill. It’s knowing your numbers - and acting on them.







Tejas Bubane
December 8, 2025This article is basically just saying don't take aspirin unless you're already dying. No shit. I've been telling my dad for years he doesn't need it. He's 68, healthy, takes a walk twice a week. He's on statins. Why would he risk a bleed for a 12% reduction in a nonfatal heart attack? The real problem is doctors still prescribe it like it's vitamin C.